Osteomyelitis
Synonyms
- endogenous osteomyelitis
- Augmentation of bone
- Inflammation of the bone marrow
- Osteitis
- Brodie's abscess
- Childhood osteomyelitis
English: osteomyelitis
definition
Osteomyelitis (plural osteomyelitis) is an infectious disease of the bone.
It is often referred to as chronic bone augmentation.
Osteomyelitis (dilated bone) can be caused by specific infections such as tuberculosis and many more. be evoked. However, osteomyelitis is usually based on unspecific infections that can be bacterial caused by open bone fractures and operations. The fact that pathogens are washed in via the bloodstream is usually just as seldom as the forwarding of neighboring foci of infection. In addition to these bacterial osteomyelitis, osteomyelitis can, in rare cases, be caused by viruses and fungi.

In the field of Osteomyeltites, that is caused by unspecific infections, a distinction is made between acute osteomyelitis and chronic osteomyelitis (chronic bone suppuration).
The acute osteomyelitis occurs in two different forms. One distinguishes between:
- the endogenous - hematogenous form (= primarily localized in the medullary canal; general disease with manifestation in the organ)
- the exogenous form (= post-traumatic, post-operative; osteitis),
which can be discussed more explicitly below.
Also the chronic osteomyelitis occurs in two different forms. A distinction is made here between:
- the secondary chronic form
- the primarily chronic form.
Acute osteomyelitis can, irrespective of whether it is endogenous - hematogenous or exogenous, become chronic if the therapy is inadequate (= secondary chronic form).
causes
In general, it can be said that almost all inflammatory diseases of the bone can be traced back to infections with various pathogens. As a rule, these pathogens are bacteria.
The spectrum of pathogens always depends on the type of infection. In most cases, Staphylococcus aureus is the spectrum of pathogens. In addition, Pseudomonas aeroginosa, Klebsiella, Staphylococcus albus, streptococci, meningococci, pneumococci and Escherichia coli can play a decisive role.
Streptococci are actually only relevant as a pathogen spectrum in hematogenic osteomyelitis in infancy and childhood.
As mentioned earlier, there are two ways that acute osteomyelitis can develop.
Either it is an endogenous - hematogenous osteomyelitis, then the pathogens are passed on via the blood from a focus of infection outside the bone, or it is a so-called exogenous osteomyelitis, then infections are passed into the body via open wounds (accidents, Operations).
Foci of infection of an endogenous - hematogenous osteomyelitis can be, for example, sinus infections (= sinusitis), tonsillitis (= tonsilitis), tooth root inflammation, boils, etc.
Read more on the subject at: Inflammation of the bone or periosteum of the heel
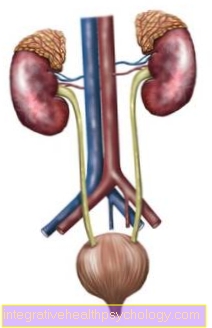
Childhood osteomyelitis
The acute hematogenous osteomyelitis is a typical disease in childhood especially between the ages of 3 and 15. Osteomyelitis in infancy or childhood usually occurs in Area of the long femur (Femoral metaphysis) on. The disease spreads under the periosteum out (subperiostal) and can get into the Bone marrow or over Vascular connections in the Spread the adjacent joint. Acute symptoms occur with fever, chills, severe local pain, swelling, reddening, overheating and relieving postures.
As Osteomyelitis causative agent so-called gram-positive pathogens (e.g. Staphylococcus aureus, Streptococci of group A) in the foreground. That is also what the targeted pathogen-sensitive antibiotic therapy the disease. In principle, hematogenous osteomyelitis should be considered in small children with pain in the extremities, redness and swelling, and if the general condition is poor. If osteomyelitis is suspected in infancy or childhood, a clinical examination the osteomyelitis disease using imaging (roentgen, Ultrasonic, Magnetic resonance imaging) diagnosed or excluded.
Diagnosis of osteomyelitis
In general, care must be taken with general infections, as the hematogenous endogenous - Osteomyelitis occurs after general infections. An infection of the umbilical cord, for example, is typical for the development of endogenous hematogenous osteomyelitis in infancy.
Occur in investigations of the Osteomyelitis For example, the symptoms already mentioned above appear, one can expect from an acute case of inflammation of the Bone go out.
The disease can also be detected in the blood. The increase in the concentration of white blood cells (= Leukocytes; Leukocytosis), as well as a significantly increased sedimentation rate (= BSG). This diagnosis of osteomyelitis is only important in the case of an acute form, since in the case of chronic osteomyelitis both values show only a moderate increase.
In the case of acute osteomyelitis, the Diagnosis In addition, the pathogen can be detected by creating a blood culture or puncturing the inflamed bone. This then gives important information about the therapeutic measures in the context of antibiosis. This has to be specific to the pathogen in order to be effective.
The x-ray diagnosis of osteomyelitis usually only becomes visible at a more advanced stage. Bone changes usually only become visible two to three weeks after the onset of the disease. Then, however, there are visible changes (see X-ray image) in the form of calcifications (= Ossifications), lighter spots and / or periosteum detachments from bone.
If the osteomyelitis is chronic, the blood vessel blockage can lead to a reduced blood supply to the bone, which under certain circumstances can even degenerate into a bone infarction. The result of a bone infarction is the death of certain bone parts, which are then called Residual body (= Sequester) remain in the infected area. X-ray diagnostic this can be seen as a light border, since dead bone tissue is usually answered by the formation of new bone tissue. The light edge is therefore connective tissue.
Furthermore, the diagnosis of osteomyelitis can be done using Sonography (= Ultrasound examination) can be diagnosed. It should be mentioned positively that, for example, the periosteum detachment from the bone, which is due to the Abscess formation is caused to be seen earlier than in the X-ray image.
So-called skeletal scintigraphy can be used as a further diagnostic measure for osteomyelitis. This diagnostic method is made possible by the very weak radioactive preparations (= Radiopharmaceuticals) evidence of inflammatory processes.
-> Continue to the topic of osteomyelitis therapy
roentgen
By Imaging procedures the osteomyelitis can be made visible. However, in acute osteomyelitis there are changes in the bone structure only recognizable in the X-ray after about one to two weeks. The further course of the disease will show up in the x-ray blotchy highlights, Detachment of the periosteum from the bone and calcifications (Ossifications). Often with chronic osteomyelitis, one develops Part of the bone dieswhich remains as a residual body (sequester) and forms in the vicinity of these bone parts new bone tissue. The resulting connective tissue around the rest of the body is in the X-ray image visible as a light border.
therapy
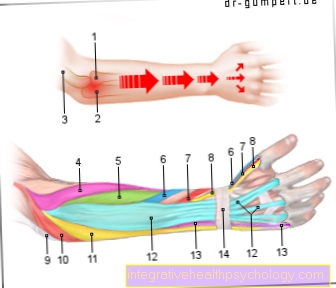
Becomes the diagnosis of osteomyelitis at a very early stage posed, so is conservative therapy with targeted antibiotic therapy and immobilization possible. There is a Smear from the puncture the focus and the causative agent of the disease is determined. A specific antibiotic therapy carried out until the inflammation parameters in the Blood count normalize. Also is on a adequate pain therapy (Analgesia) to be observed.
However, it is often necessary to have a rapid surgical intervention to renovate the stove. The Bone drilled to relieve pressure (Bone trepanation), rinsed extensively and the damaged bone areas removed. Often will Antibiotic carriers insertedin order to achieve locally high levels of the antibiosis. Depending on Degree of severity of the defect in the bone may need Bone grafts and several follow-up operations are performed. Just by one prompt therapy osteomyelitis can heal without Bone or joint damage can be achieved. Often the therapy of osteomyelitis is one lengthy process.
Therapy of osteomyelitis
A distinction must be made between the endogenous - Haematogenous osteomyelitis in infants, children and adults.
The therapeutic treatment of the Osteomyelitis in infancy occurs through the administration of Penicillins according to the spectrum of pathogens and by immobilizing the affected body region using a splint or plaster cast. Is a joint Affected by osteomyelitis, this joint is usually flushed. This can work in several ways:
- by Puncture or
- through a so-called Irrigation - suction - drainage.
In the event that the osteomyelitis has progressed so far that the growth plate has already been damaged, secondary reconstructive measures may be necessary.
The therapeutic treatment of the Osteomyelitis in childhood is done via targeted Administration of antibiotics in connection with immobilization using a splint or plaster cast of the corresponding body region. In very special cases, for example if residual bodies or abscesses form, surgical intervention may be necessary. Only in rare cases is there a transition from the acute to the chronic form Osteomyelitis.
The therapy in adulthood also takes place via a targeted administration of antibiotics in connection with immobilization using a splint or plaster cast. In contrast to infancy or childhood, the bacterial foci of osteomyelitis are cleared out early in adulthood. If necessary, removed Bone parts by so-called Cancellous plasty (= Transplantation of bone substance from another, endogenous, healthy one bone) must be replaced so that the functionality of the relevant limb can be maintained. In addition, in Tehrapie Irrigation - suction - drainage inserted to flush out foci from the affected joints. In contrast to acute osteomyelitis in children, in adults there is often a recurrence and transition to the chronic form of osteomyelitis.
Complications:
As already mentioned, there is a risk in infancy and childhood that the acute inflammation will damage the growth zone (= metaphysis) of the affected bone. This damage can then under certain circumstances cause severe deformities or shortening of the affected extremities.
There is a particular risk with osteomyeltitis up to the age of 2. The blood vessels of the Medullary canal run at this age directly from the metaphysis (= growth zone of the bone) through the cartilaginous epiphyseal plate into the epiphysis (= end piece of the bone; transition to the joint). As a result, the pathogens can also penetrate the joints and cause purulent joint effusions there, which in turn can cause severe joint damage and possibly even growth disorders.
Every acute endogenous hematogenous osteomyelitis, especially in adult patients, carries with it the risk of developing into the chronic form. Then there are considerable remodeling processes within the affected bone, under certain circumstances bone infarctions can occur, whereby certain parts of the bone are no longer supplied with blood and die. The dead bone parts then remain as residual bodies (= sequesters) in the infected area. In addition, reactive connective tissue formation (= osteosclerosis) occurs, which decreases the elasticity of the bone and increases the risk of bone fractures. Adults in particular are prone to recurrence.
Antibiosis
Crucial for that antibiotic treatment osteomyelitis is that Pathogen detection at the affected area. In any case, one should Blood test done , possibly also a Puncture of fluid retention and Abscesses at the osteomyelitic focus in order to be able to determine pathogens. Treatment with antibiotics is done in the best case, pathogen-specific, immediately and will administered intravenously. In the acute inflammatory phase of osteomyelitis, it is crucial that the antibiotic long enough to the site of the infection is brought. In addition, the concentration of the antibiotic at the site of action must be sufficient to prevent the Kill pathogens efficiently. As with any targeted antibiotic, this is important best possible testing for resistance of the pathogen against various antibiotics. Treatment with the antibiotic Clindamycin has been shown to be beneficial as it is effectively accumulates in the bone area and a complete cure of the disease can be achieved. Alternatively, a Antibiosis with penicillins (e.g. oxacillin, flucloxacillin) or cephalosporins. Usually antibiotic therapy can be stopped when the Sedimentation rate (ESR, unspecific inflammation parameter) normalized or symptom-free.
Just that targeted antibiosis prevented Transitions to chronic osteomyelitis. Chronic osteomyelitis, on the other hand, usually requires one surgical intervention.
Endogenous osteomyelitis
As already under causes described, an endogenous - hematogenous osteomyelitis develops due to pathogens that enter the body via the blood from a specific focus of infection Bone marrow one Bone is abducted. There they then settle, which makes it Abscess formation comes.
Abscesses are foci of pus that the body can intercept with very good to good immune defenses. Then they remain locally limited, while with a poor immune status they often spread.
As you can see from this, the Course of the disease of individual factors, such as the Immune defense, but also that Age dependent on the patient.
With children Until the age of two, blood vessels of the medullary canal run directly from the metaphysis (= growth zone of the bone) through the cartilaginous epiphyseal plate into the epiphysis (= end piece of the bone; transition to the joint).
As a result, the pathogen also enters the Joints can penetrate and cause purulent joint effusions there, which in turn causes severe Joint damage, possibly even Stunted growth may occur.
With increasing age, im Childhood and Adolescence the blood flow to the epiphyseal plate from until it is later no longer supplied with blood. Thus the infection of the Bone marrow always limited to the metaphysis, so that the joints are then usually no longer affected.
The exception to the rule, however, is this hip joint, since the metaphysis in the gel capsule is included there. Thus, the joint can also be affected here.
However, as soon as the end of the growth phase has been reached, the cartilaginous components ossify. This removes the protective border to the epiphyseal plate again. As a result, infections of the joints can recur in adults - similar to children up to two years of age.
In addition to the individually different course, the Virulence (= aggressiveness) of a pathogen affects the course of the disease. As a result, one and the same type of pathogen can cause different types of the disease.
The spectrum then fans out from one mild illness with mild complaints up to acute sometimes lsimilar complaints, or chronic course in chronic osteomyelitis.
There are forms of endogenous - hematogenous osteomyelitis, which are often chronic.
These are for example the so-called Brodie abscess, of the Paget's disease or the tuberculous osteomyelitis (see: definition).
Each of these diseases occurs very rarely compared to the other forms, but all have an individual clinical picture with very typical, individual disease patterns and courses.
frequency

According to scientific surveys, endogenous osteomyelitis occurs predominantly in children and adolescents, with a specific accumulation in the eighth year of life, mostly after a general infection. Mostly the thigh or tibia was (Femur and Tibia) affected by the disease. On average, boys seem to be more frequently affected by the disease than girls.
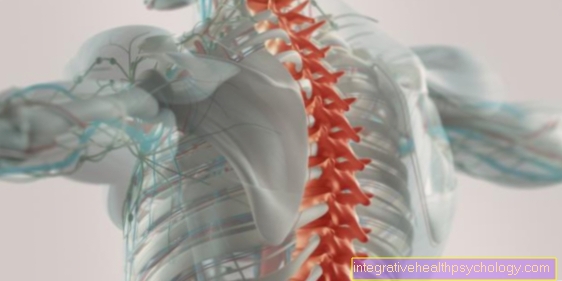
With regard to endogenous osteomyelitis in adulthood, it can be stated that this disease is rather rare. As in childhood and adolescence, men are more often affected than women. The endogenous - hematogenous osteomyelitis includes in adulthood in addition to the long Long bones (e.g. tibia bone = tibia) also the Spine.
Symptoms
The endogenous - hematogenous osteomyelitis In infancy and toddlers, it usually proves to be a disease of the entire body and usually manifests itself with a fever of up to approx. 40 ° C. In addition, depression and chills become noticeable. Areas affected by the Inflammation of the bones are affected by severe redness, swelling and tenderness.
The symptoms mentioned are usually less noticeable in adults. Typical symptoms are depression, pain and functional restrictions in the affected areas. The inflammation of the corresponding area can become noticeable through a slight overheating (possibly also redness), but this type of symptoms are significantly less pronounced in relation to infants and toddlers.
As already mentioned several times, such a disease can sometimes become chronic. Then the pain in the affected areas, including the functional restrictions, are in the foreground.
Forecast:
In the case of acute hematogenous infant osteomyelitis, the chances of recovery are earlier therapy Well. In cases in which the disease has already progressed and has caused destruction of the growth plate, sometimes considerable growth disturbances can occur.
Even with one acute hematogenous osteomyelitis in childhood, the prognosis depends considerably on the damage to the growth plate. Here, too, considerable bone damage can sometimes occur, which under certain circumstances can lead to shortened extremities.
-> Continue to the topic of osteomyelitis diagnostics
The same applies to an acute endogenous - hematogenous osteomyelitis in adulthood:
If the disease is recognized in good time and subsequently treated consistently, healing is usually possible without permanent damage. However, there is a risk that the disease - unless it is recognized early and treated appropriately - will turn into one chronic osteomyelitis transforms.
In comparison to the acute form, chronic osteomyelitis is difficult to treat and tends to flare up again (renewed infection of the bone) even if the healing process is successful.
The genesis:
Under one exogenous osteomyelitis one understands bone marrow inflammation, which is either due to an open wound after an accident (= post-traumatic) or as part of a surgery (= postoperatively) arises. In both cases it is essential Germs from the outside and spread in the wound area in such a way that initially a local inflammation within the Bone arises. As with the endogenous - hematogenous osteomyelitis are among the main pathogens Staphylococcus aureus, but also Escherichia coli and Proteus. Other bacterial pathogens can also trigger the disease.
The course of the disease is very individual and depends on various factors. The extent to which pathogens can spread in bones and also spread from there depends primarily on a patient's individual immune defense. This means that especially patients with a reduced immune defense (for example after a transplant, caused by a so-called immunosuppressive therapy) of acute, but also chronic disease courses Osteomyelites are affected.
Patients who have insufficient blood flow to the bone are also at risk. This is the case, for example, with patients who have Diabetes mellitus (= Diabetes) or under arteriosclerosis (= Hardening of the arteries) Suffer.
Frequency:
Due to the history of origin (post-traumatic, post-operative) exogenous osteomyelitis, it is understandable that this disease occurs predominantly in adults.
According to statistical surveys, men tend to be more frequently affected by accidents than women, so that one can conclude that men are more frequently affected by this disease than women.
Symptoms:
In the acute form of the exogenous postoperative Osteomyelitis you can see the first symptoms three to four days after the operation. The patient usually responds with it fever, Swelling and redness of the affected area and possible wound secretion. Patients also often complain of pain and depression.
Similar symptoms appear in the post-traumatic osteomyelitis.
In such cases, action must be taken quickly to make the transition into the secondary - chronic osteomyelitis to prevent.
Diagnosis:
The occurrence of the above-mentioned symptoms in combination with a traumatic experience or as a result of an operation allows the conclusion that exogenous osteomyelitis is present.
A further diagnosis is usually made via an Blood analysis. The inflammation barometer is the CRP value measured, as well as the sedimentation rate (BSG), which is significantly increased in the case of osteomyelitis. An increase in the white blood cell concentration (= Leukocytes; Leukocytosis). These diagnostic measures are only of importance in the case of an acute form, since in the case of chronic osteomyelitis both values show only a moderate increase
The x-ray diagnosis of osteomyelitis usually only becomes visible at a more advanced stage. Bone changes usually only become visible two to three weeks after the onset of the disease. Then, however, there are visible changes (cf. X-ray image) in the form of calcifications (= ossifications), lighter spots and / or periosteum detachments from the bone.
If the osteomyelitis is chronic, it can lead to a reduced blood supply to the bone due to blood vessel blockages, which may even lead to a Bone infarction can degenerate. The result of a bone infarction is the death of certain bone parts, which are then called Residual body (= Sequester) remain in the infected area. In the X-ray diagnosis, this can be seen as a light border, since dead bone tissue is usually answered by the formation of new bone tissue. The light edge is therefore connective tissue.
Furthermore, sonography (= Ultrasound examination) can be diagnosed. It should be mentioned positively that, for example, the periosteum detachment from the bone, which is caused by the abscess formation, can be seen earlier than in the X-ray image.
So-called skeletal scintigraphy can be used as a further diagnostic measure. This diagnostic method is made possible by very weak radioactive preparations (= Radiopharmaceuticals) evidence of inflammatory processes.
Therapy:
Therapeutically, it is possible to respond both conservatively and surgically. Due to the poor local blood circulation, conservative antibiotic therapy has little prospect of a cure, since only an insufficient concentration of active ingredient can be achieved at the intended location.
For this reason, a present exogenous osteomyelitis usually surgically responds. You can proceed in different ways, the following should be mentioned here as an example:
- The operative radical removal of the focus of inflammation, possibly combined with Cancellous plasty (= Transplantation of bone substance from another, endogenous, healthy bone), flushing and drainage.
- The inlay of irrigation - suction - drains.
- Systemic antibiotic therapy over a period of one to about one and a half months.
Complications:
Exogenous acute osteomyelitis can degenerate into a serious disease of the entire body and - in unrecognized cases - even sepsis (= Blood poisoning), which in turn can have serious consequences, such as organ damage.
Quick action in the event of a exogenous acute osteomyelitis is required because the transition to secondary chronic osteomyelitis is fluid. Chronic osteomyelitis has far less chance of a cure and can lead to pronounced bone remodeling processes and even to bone stability disorders as a result of bone infarcts.
It is also possible for the disease to spread to neighboring joints, which can lead to significant restrictions on movement, and in severe cases even stiffening and shortened limbs (Amputations) occur as a consequence.
Prognosis for exogenous osteomyelitis
If the disease osteomyelitis is detected early, there is a chance that it will heal without any remaining damage. As already mentioned, the therapy is usually surgical, since the conservative one Antibiotic therapy seldom works due to poor blood circulation in the bones. Since the transition to the secondary - chronic form of osteomyelitis is fluid, healing often proves to be difficult (see above). The chronic osteomyelitis tends to recur even after healing has been successful, so that the disease can flare up again and again.