Spinobulbaris tract
Synonyms
Medical: Substantia alba spinalis
CNS, spinal cord, brain, nerve cell, gray matter spinal cord
English: spinal cord
introduction
This text tries to explain the very complex relationships in the spinal cord in an understandable way. Due to the complexity of the topic, it is aimed at medical students, doctors and very interested laypeople.
Explanation
The spinobulbaric tract is divided into:
- Gracilis fasciculus (GOLL) and
- Fasciculus cuneatus (BURDACH)
These two tracts lie in the posterior cord of the white matter of the spinal cord (funiculus posterior). As an ascending (afferent) pathway, they lead from the spinal ganglion to two nuclear areas that lie in the elongated medulla (medulla oblongata): the gracilis fasciculus to the “graceful nucleus”, the Ncl. gracilis, and the cuneatus fasciculus to the Ncl. cuneatus. (Ncl. = Nucleus = nucleus). This is where the first central switchover point is located, the second neuron of the posterior strand.
The two tracts are therefore summarized as the spinobulbar tract, ie "tract from the spinal cord to the nuclei", because they convey the same information, namely sensation of touch and sensation of vibration (the so-called surface or epicritical sensibility) as well as our sense of the position of our muscles and Joints (and therefore of the whole body) in space and also to each other (= sense of position, depth sensitivity, sense of strength or proprioception).
The cuneatus fasciculus carries the information from the upper half of the body, i.e. it consists of extensions of dorsal ganglion cells of the neck and upper chest segments.
The gracilis fasciculus carries the information from the lower half of the body, i.e. it consists of extensions of the dorsal root ganglion cells of the lower thoracic as well as the lumbar and sacrum segments.
The border between the two is approximately at the level of the breast segment 5 (Th 5), but this is individually different.
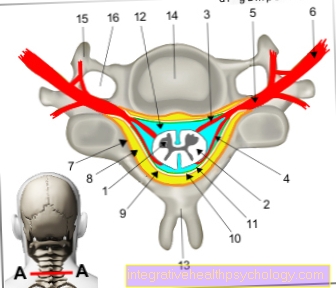
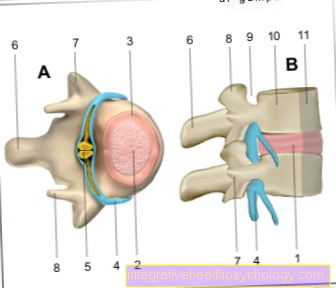
Figure spinal cord

1st + 2nd spinal cord -
Medulla spinalis
- Gray matter of the spinal cord -
Substantia grisea - White spinal cord substance -
Substantia alba - Anterior root - Radix anterior
- Back root - Radix posterior
- Spinal ganglion -
Ganglion sensorium - Spinal nerve - N. spinalis
- Periosteum - Periosteum
- Epidural space -
Epidural space - Hard spinal cord skin -
Dura mater spinalis - Subdural gap -
Subdural space - Cobweb skin -
Arachnoid mater spinalis - Cerebral water space -
Subarachnoid space - Spinous process -
Spinous process - Vertebral bodies -
Vertebral foramen - Transverse process -
Costiform process - Transverse process hole -
Foramen transversarium
You can find an overview of all Dr-Gumpert images at: medical illustrations
function
The spinal ganglion cells have their receiving (dendritic) ends wherever they get the "sensitive information", e.g .:
- in the skin
- in the subcutaneous tissue
- in the joint capsules
- the periosteum
- the cartilage
- the muscle fascia and
- the tendons.
Nerve cell

- Dendrites
- Cell body
- Axon
- Cell nucleus
These dendritic ends are called "free nerve endings".
In addition to them, there are also specialized receptors such as the so-called. Merkel cells the skin or the Meissner tactile bodies, the Golgi tendon organs or the muscle spindles.
The stimulus that these endings register, e.g. a stretching stimulus of the tendon, is directed to a peripheral nerve Spinal nerves (Spinal cord nerves) of a segment and from here to the spinal ganglion cell, which is the first neuron of this pathway.
This neuron is pseudounipolar. The impulse that arrives now runs through the posterior root (radix posterior) into the spinal cord. The signal forwarding is divided here:
- on the one hand as a long branch in the said (spinobulbar) path to the core areas Ncl. gracilis or Ncl. cuneatus (depending on the level at which the stimulus arose),
- on the other hand, as short branches to intermediate neurons (so-called. Axon collaterals) of the rear horn or
- directly to motor cells of the anterior horn, creating a simple Reflex path arises.
But let's take a look at the long ascending branch, the actual Hinterstrangbahn.
The gracilis fasciculus and the cuneatus fasciculus run up to their associated nuclei on the "same" (= ipsilateral) side, which means that the sensations (touch, vibration, sense of position) come from the left foot and the left hand also on the left im Spinal cord run away.
Both on their way and in the nuclei themselves there is a strict somatotopic structure, which means that every location in the periphery has an exact local representation at all stations of its path up to the cerebral cortex:
the further down the segment into which the stimulus information enters, the further sideways in the path it runs.
In the two nuclei, the fibers are each switched to a second nerve cell, which their extensions to the Thalamus in the Diencephalon sends.
They are no longer called "Spinobulbaris“Because they left both the spinal cord (spino-) and the nuclei (bulbi) behind. These fibers now cross each other on the other side, i.e. they run contralateral. The fibers that now run to the left carry the information from the right half of the body. They are called on this section Lemniscus medialis, the "loop further in the middle", and are part of a pathway that leads nerve fibers from different core areas to the thalamus (Bulbothalamic tract).
That is why the web is called that from here on lemniscale system designated. In a certain core area of the thalamus (Nucleus ventralis posterolateralis) they will be on their third Nerve cell switched, which sends its processes to the cerebral cortex, there in the Postcentral gyrus. This is the turn of the brain that lies directly behind the central furrow and is, so to speak, a “terminal point” for all sensitive information.
Some fibers of the sense of position that Proprioception, also end in other core areas, especially the Nucleus thoracicus dorsalis (also called Stilling-Clarke column), which can be found in the rear horn at the level of segments C8-L3.
From there they'll be over the posterior cerebellar lateral cord tract (= Tractus spinocerebellaris posterior) to Cerebellar cortex sent.
Diseases
If the posterior cord is damaged, what is known as posterior cord ataxia occurs. Here, movements are uncoordinated and the gait pattern is very insecure, the patients have a clear tendency to fall because the information about the position of the joints and muscles in space is no longer adequately passed on and the extent of movements can no longer be correctly estimated by the brain. The unconscious “counter-steering” of the body can therefore no longer function properly.
Because the fibers that carry this information cross late (in the brain stem) to the opposite side, patients have a tendency to fall to the side where the damage is in the spinal cord (ipsilateral).
In addition, there is a lack of a sense of vibration (so-called pall anesthesia) and the ability to recognize objects by touching them with the hands when the eyes are closed (stereoagnosis).
The ability to perceive two simultaneous stimuli on the skin as being in different places (two-point discrimination) is also reduced or absent.
Causes for the damage to the posterior strand can be:
- Last (4th) stage of syphilis (tabes dorsalis)
- Funicular myelosis (destruction of the nerve sheaths with vitamin B 12 deficiency)
- Spinal cord tumors
- Occlusion of the posterior spinal arteries