What is partial anesthesia?
In contrast to general anesthesia (general anesthesia), partial or regional anesthesia only numbs a certain area of the body.
In this region, pain perception, sensation and sometimes also the ability to move are switched off with the help of different procedures.
Partial anesthesia alone may be sufficient for minor interventions. For larger, more extensive procedures, it can be combined with general anesthesia.
Depending on the procedure, the anesthetist (anesthetist) can use different methods of partial anesthesia.
For example, infiltration anesthesia / surface anesthesia ("local anesthesia"), blockade of peripheral nerves (conduction anesthesia), procedures close to the spinal cord (epidural / epidural anesthesia, spinal anesthesia or combined procedures) or intravenous regional anesthesia.
Read more about this under: Short anesthesia

Reasons for partial anesthesia
Partial anesthesia is used to treat pain during and after surgery or as part of obstetrics.
In particular, it is becoming increasingly important in pain therapy during and after the procedure.
Reasons for a partial anesthetic are e.g. Operations that do not necessarily have to be performed under general anesthesia, the refusal of general anesthesia by the patient or a high risk during the procedure for seriously ill patients.
If operations are performed that require the cooperation of the patient during the procedure, partial anesthesia is also necessary, as the consciousness and possibly also the mobility are retained. Local or regional anesthesia is also preferable for patients who are not fasting because the protective reflexes are retained here (cough reflex, etc.).
This means that the risk that stomach contents will run back and enter the windpipe / lungs (aspiration) is much lower. However, if the procedure is extensive, e.g. after a serious traffic accident with multiple injuries, general anesthesia is unavoidable.
In alcoholic patients there are some advantages of partial anesthesia due to the increased risk of complications and altered metabolism. There is also the option of combining general and partial anesthesia.
Even in older patients, partial anesthesia is sometimes more beneficial and associated with significantly fewer after-effects. More about this on our website: Anesthesia in the elderly
The individual stages of anesthesia and the associated risks can be found under: Stages of anesthesia
Where can you do partial anesthesia everywhere?
A partial anesthetic can be used in many ways.
For example, for interventions in gynecology and obstetrics (often epidural or spinal anesthesia for caesarean section or vaginal delivery).
Partial anesthesia is also often used for operations on the extremities (arms / legs). This is especially true for interventions on the shoulder joint or when implanting a new knee or hip joint. When implanting (“inserting”) a new knee or hip joint as a combination with general anesthesia.
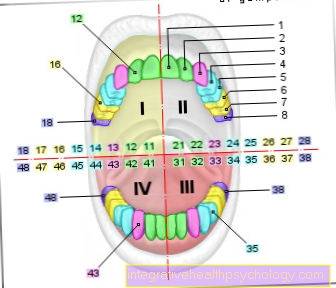
Dental treatments are also often carried out with “local anesthesia”, i.e. infiltration anesthesia. Intravenous regional anesthesia is suitable e.g. for short interventions in the area of a foot or hand.
Read more on the subject under: Epidural anesthesia and regional anesthesia
Partial anesthesia on the arm
Different methods are used depending on which procedure is to be performed on the arm.
Possible options include arm plexus anesthesia ("plexus brachialis blockade"), intravenous regional anesthesia or local anesthesia (local anesthesia) of the area to be anesthetized.
With local anesthesia, the local anesthetic ("local anesthetic") is e.g. injected into the area of the wound edges around a cut under the skin.
In intravenous regional anesthesia, after the blood is smeared out of the arm and the arm is temporarily tied, the drug is injected into the vein and the arm is anesthetized.
With the so-called “arm plexus anesthesia” or “plexus brachialis blockade”, the nerve plexus essential for supplying the arm is numbed by an injection following local anesthesia.
Read more on the subject under: Local Anesthesia and Peripheral Nerve Block
Partial anesthesia on the leg
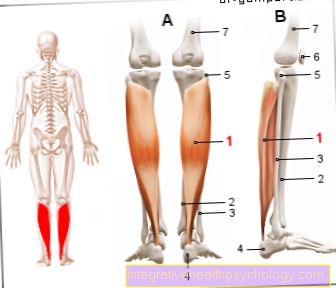
There are various options for partial anesthesia in the area of the legs.
With local anesthesia, a local anesthetic is injected superficially under the skin. There is also intravenous regional anesthesia.
First, the blood is smeared from the corresponding leg, so that a so-called "blood void" arises.
The leg is then tied off and the anesthetic is injected into the appropriate vein.
After the procedure, the air-filled cuff is slowly opened to bind it. With a peripheral nerve block, anesthetic is injected into the area around the nerve in question. The “sciatic nerve” (sciatic nerve) and the femoral nerve with their respective divisions are essential for supplying the leg.
Read more on the subject under: Sciatic nerve and femoral nerve
Femoral catheter
A partial anesthetic using a so-called femoral catheter is used as follows.
- First, the femoral nerve is found in the groin area using ultrasound.
- Possibly. the correct position is also checked with an electrical nerve stimulator.
- If the tip of the needle is correctly positioned, the quadriceps femoris muscle twitches (front of the thigh, movement in the area of the kneecap, etc.).
- Then the thin tube (the pain catheter) is inserted, fixed and the local anesthetic is injected over it.
- In addition to the actual procedure, local anesthetic can be administered via this catheter.
- This means that fewer painkillers that work throughout the body (tablets, intravenous syringes, etc.) are required.
- The catheter can be removed after a few days.
Read more on the topic under: Femoralis Catheter
Spinal anesthesia
Spinal anesthesia / lumbar anesthesia is one of the spinal cord-related procedures of partial anesthesia or the central line anesthesia.
The aim is to achieve a safe, fast and reliable blockade / anesthesia of the spinal nerve roots.
As a result, the sensation of pain, the sensation of touch, the ability to move and the effect of the sympathetic nervous system in the area to be operated on are reversibly (reversibly) switched off.
The puncture site is below the third lumbar vertebra. Here, bathed in brain water / nerve water (liquor), “only” the roots of the spinal nerves are located.
In the area above, however, is the compact spinal cord. It is therefore safe to puncture below the third lumbar vertebra.
After thorough disinfection and local anesthesia, the patient is asked to bend his back into a so-called "cat hump" (rounded back).
The puncture needle is advanced through the hard meninges (dura mater) into the so-called subarachnoid space / liquor space. Then the local anesthetic is administered. During the entire procedure, the patient is constantly monitored (EKG, blood pressure measurement, pulse measurement, measurement of oxygen saturation).
Usually there is initially a feeling of warmth immediately after the puncture and injection of the anesthetic. Senselessness, freedom from pain in this area and inhibition of mobility follow within a few minutes.
The spread of the anesthetic and the duration of the spinal anesthesia depend directly on the patient's position (influence of gravity), the choice of drug (different density) and the dose.
Depending on the selection and control of this type of anesthesia, the partial anesthesia can spread to the thoracic vertebral area, making it possible to perform many different operations.
Read more on the subject under: Spinal anesthesia
Partial anesthesia for a caesarean section
Two methods of partial anesthesia can be used for a caesarean section (Sectio caesarea).
A spinal or epidural anesthesia (PDA) (synonym: epidural anesthesia).
With both methods, the pregnant woman remains conscious. In contrast to the rarely used general anesthetic, this enables her to see her newborn in the operating room immediately after the birth.
In the case of spinal anesthesia, the local anesthetic is injected directly into the room in which the cerebral water / nerve water is located.
With epidural or epidural anesthesia, the syringe is "only" pushed into the epidural / epidural space.
This is a space that is physiologically present in the area of the spine and is formed by the inner and outer sheets of the hard meninges. If a particularly rapid onset of action is required, spinal anesthesia is usually preferred. In the case of epidural or epidural anesthesia, a so-called pain catheter can be inserted and fixed. Painkillers can also be administered to this region after the procedure.
Read more on the subject under: epidural anesthesia, epidural anesthesia and anesthesia during pregnancy
Advantages of partial anesthesia
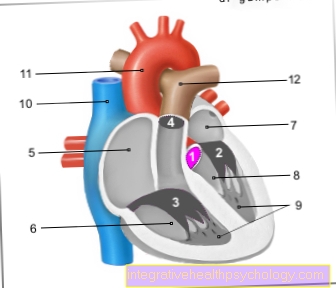
The advantages are, among other things, that various important body functions / organ systems are significantly less stressed compared to general anesthesia. For example, partial anesthesia is particularly suitable for patients with chronic lung disease (e.g. COPD).
They benefit from not using ventilation during the operation. The body's metabolism and acid-base balance also have to compensate less. This can be a reason for chronically and / or multiply ill patients, e.g. With
- Diabetes mellitus ("diabetes"),
- Heart failure ("heart failure") or
- Operation under general anesthesia after a heart attack.
The consciousness is not impaired, apart from any sedation (twilight sleep) carried out.
Artificial ventilation, including the administration of muscle relaxants, is also not required.
As a rule, no high doses of systemically effective painkillers (drops, tablets, intravenous syringes) are required immediately after the procedure, as e.g. the anesthesia of the relevant extremity (arm, leg) already provides good pain relief.
The procedures of partial anesthesia usually not only work during the operation, but also significantly beyond. Because of this, pain medication can be saved in the postoperative period. Depending on the patient and the procedure, so-called pain catheters (e.g. PDK = epidural catheter) can also be placed.
These are connected to a pump system. Blocking times and dosing are set. Then the patient can "re-inject" pain medication several times a day at the push of a button.
Side effects and risks of partial anesthesia
These are very safe, routinely used standard procedures.
Nevertheless, bleeding complications with the formation of a hematoma can occur with all procedures.
The bleeding / hematoma can compress the surrounding structures, especially nerves, and lead to failure symptoms.
Allergic reactions can occur in the event of intolerance to medication. Infections after the procedure are also possible.
With the procedures near the spinal cord, back pain can also occur due to the puncture.
Puncturing the hard meninges during spinal anesthesia can cause a small leak and loss of cerebrospinal fluid.
This leads to negative pressure and so-called "post-puncture headaches". This can be treated well with targeted treatment.
You can also
- Nausea,
- Vomit,
- Blood pressure fluctuations and
- Cardiac arrhythmias occur.
- Urinary retention (inability to spontaneously empty the urinary bladder) is a possible complication but can be treated well.
The most serious complication, which occurs extremely rarely, is the so-called total spinal anesthesia. This can occur if the local anesthetic is accidentally overdosed, if the anesthetic rises too high in the cerebral fluid or if the injection needle is accidentally positioned in the subarachnoid space instead of the epidural space. With total spinal anesthesia it comes to
- Unconsciousness,
- Respiratory and cardiac arrest.
Thanks to the permanent presence of an anesthetist and a professional team, as well as numerous monitoring options, help can be provided quickly even in such a situation.
Read more on the subject under: After-effects of anesthesia, complications in anesthesia and risks of anesthesia
Which drugs or resources are used?
So-called "local anesthetics" (local anesthetics) are usually used for partial anesthesia. These work by penetrating into the area of the corresponding nerve after injection and blocking the so-called "voltage-controlled sodium channels" there, which are responsible for the transmission of pain.
However, they work much worse in inflamed tissue due to the changed environment. Therefore, due to the weakened effect and the additional risk of infection, no injection should be made into inflamed areas.
There are different preparations that differ in their duration of action and are selected depending on the duration of the procedure. In addition, depending on the area, adrenaline can be added.
This causes the vessels to contract and thus has a hemostatic effect.
Do you have to be sober for partial anesthesia?
Since every procedure and every patient is individual, the anesthetist responsible will determine in advance how many hours before the operation you can smoke, eat and drink the last time.
In principle, partial anesthesia can also be used as the sole anesthetic procedure for patients who are not fasting.
However, with every procedure there is a risk that complications may require general anesthesia. Therefore, just like before a general anesthetic, the patient should be sober. This avoids complications if general anesthesia has to be performed during the procedure.
What are the alternatives to partial anesthesia?
The superficial, local anesthesia, which does not count as anesthesia / partial anesthesia, can be an alternative.
However, only if the intervention allows it, e.g. for sewing smaller cuts in the area of arms / legs.
In addition, for endoscopic examinations (colonoscopy, gastroscopy, lungoscopy) or smaller plastic surgeries, there is the possibility of so-called analgosedation (“twilight sleep”).
The patient continues to breathe spontaneously and is monitored by means of monitoring (EKG, measurement of oxygen saturation, pulse measurement, blood pressure measurement). The consciousness is dampened somewhat, pain therapy with the help of intravenous painkillers is carried out.
Sedatives are also given to shield the patient. In addition to analgesia, both general anesthesia and a special variant of general anesthesia, the so-called total intravenous anesthesia (TIVA), are possible.
In comparison to "normal general anesthesia", TIVA does not use inhalation anesthetics and the medication is only administered intravenously. Here “only” sleeping pills (hypnotics) and pain relievers (analgesics) are used.
Certain substances with a particularly short half-life are used. This ensures that the anesthesia can be easily controlled / planned. Other advantages of this method are less nausea and vomiting, and no side effects associated with inhaled substances.