Celiac disease
Synonyms in a broader sense
Gluten-sensitive enteropathy, indigenous sprue, gluten intolerance
Alternative notation: Celiacia
Epidemiology / frequency
In Europe there is around 1 in 500 inhabitants Celiac disease ill. Women are more often affected than men.
The disease usually occurs for the first time in childhood (= first manifestation); adults get sick Celiacia, this usually happens in the 3rd and 4th decade of life.
The Gluten intolerance remains lifelong, only the so-called transient (= temporary) celiac form of childhood can regress.
10-15% of the relatives of people with celiac disease become ill or also have one Gluten intolerance ill.
Some diseases occur more frequently with that Gluten intolerance on, e.g. the Ulrich Turner Syndrome, the Trisomy 21, of the Type I diabetes mellitus or autoimmune diseases.
definition

The Celiacia is an intolerance reaction of the body to gluten and manifests itself as a digestive disorder (=Digestion) and the recording (=absorption) of the food components from the Small intestine (=Duodenum). The disturbance of digestion and absorption is collectively called Malassimilation designated.
The patients with celiac disease show an intolerance or hypersensitivity to gluten. gluten is a grain protein, a sticky protein found in:
- wheat
- barley
- rye
- oats
- Spelt or
- Green kernels is included.
If the sick eat gluten, they suffer Diarrhea, Malabsorption (= impaired absorption of food components) and weight loss due to damage to the small intestinal mucosa:
The mucous membrane of the upper small intestine is reshaped, the small intestinal villi, which are important for the absorption of food components, recede and the depth of the crypts (= tubular depressions of the mucous membrane, located between the villi) increases.
At the microscopic level, the changed small intestine now resembles the image of the Colon (= Colon), which is why one speaks of a colonization of the small intestinal mucosa in celiac disease.
Cause / origin
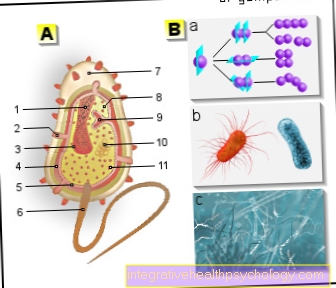
Gluten intolerance is a disease in which the immune system Antibodies (defense substances) produced against components of the own body (= autoimmune antibodies).
In the case of celiac disease, lie antibody against the Tissue glutaminase before, an enzyme (protein) that is part of many body cells.
The reaction of autoantibodies with Gliadin, a component of gluten, causes the immune system to be activated, so that inflammatory cells migrate into the mucous membrane of the small intestine and maintain an inflammatory reaction there.
The small intestinal villi, fine protrusions of the small intestinal mucous membrane that serve to absorb nutrients from the small intestine, go under (= atrophy).
Thus, the absorption of the food components from the intestine into the blood is no longer possible or severely restricted.
Symptoms of Celiac Disease
In the foreground of the symptoms of gluten intolerance / celiac disease, there are disorders of the general condition changed stool behavior and a (mostly painful) Abdominal distension (=Meteorism).
Patients feel sick, they just are limited performance and sometimes very bad-tempered. You are weakened and losing weight.
The stool has a mushy consistency, smells bad and occurs in large quantities.
The stomach of the patient is distended because the digestion of sugars (=Carbohydrates) is impaired.
The patients with celiac disease often have stomach pain and Flatulence (Flatulence) are common.
Children and Celiac Disease
The disease falls in childhood usually in the first year of life, when the transition from nutrition with Breast milk, which is gluten-free, is made to form food that contains gluten.
The little patients are often ill-tempered, have hardened expressions and suffer from diarrhea, and they also lose weight, which results in a so-called "Percentile break " makes clear:
The children develop worse in comparison to children of the same age, which is shown by a lag in their weight and possibly also in height compared to their peers.
Diagnosis of Celiac Disease
To diagnose celiac disease, a blood sample is checked for the presence of various antibodies.
A positive test for gliadin IgA antibodies (= antibodies against gliadin), endomysium IgA antibodies (= antibodies against muscle components) and for tissue glutaminase IgA antibodies (= antibodies against the enzyme tissue glutaminase of the body cells), which is the one for the sprue is the most typical and therefore most specific antibody means that these antibodies are present.
In addition, a tissue sample (= biopsy) must be taken from the small intestine and examined to confirm the diagnosis.
Special cell changes in the tissue sample indicate celiac disease:
Microscopic examinations show a reduction in the small intestinal villi and an infiltration of the mucous membrane with inflammatory cells (lymphocytes and plasma cells).
Another diagnostic criterion is the improvement in symptoms and the drop in autoantibody levels in the blood under gluten-free diets.
As part of the diagnosis of celiac disease, HLA is also determined. For more information, read the following article: HLA - Human Leukocyte Antigen - What is it?
Note diagnosis
Meet the diagnostic criteria
- the positive antibody test,
- a pathologically altered small intestinal mucosa and a
- Improvement under diet
for the patient, there is a high probability of gluten intolerance.
Symptoms that result from impaired nutrient and mineral intake are also a
- Iron deficiency with Anemia (= Anemia)
- a Vitamin B12 Loss
and - a Calcium deficiency.
therapy

There is no causal (eliminating the cause) therapy for celiac disease.
The disease is not curable, but by one gluten free diet, a so-called Elimination diet, easy to treat, so that within a few weeks there are no more symptoms. This elimination diet must be followed for life.
Gluten-free foods include:
- Potatoes
- Corn
- Rice,
- Millet and
- Soy.
Products made from wheat, oats, barley, rye, spelled or green spelled should not be consumed.
If there is a transient, i.e. Temporary celiac disease, which regresses again, it is possible to reload with gluten after a few years of therapy. This can be done when the levels of the antibodies in the blood, which serve as parameters for observing the course of the disease, have fallen.
Complications
As a concomitant disease of celiac disease, which can also be traced back to the changes in the small intestinal mucosa, the Lactose intolerance to call. It describes an enzyme deficiency in the intestinal mucosa, which can be traced back to the changes in the small intestinal mucosa that are typical of celiac disease:
The enzyme lactase breaks down double sugars into single sugars in the cells of the mucous membrane of the small intestine. The body can only absorb carbohydrates in the form of simple sugars. If the mucous membrane lacks lactase, carbohydrates are not absorbed. Patients with celiac disease should therefore refrain from consuming lactose until the mucous membrane of the small intestine has regenerated.
Prognosis and course
Patients with celiac disease should follow a gluten-free diet, otherwise their risk of developing a malignant lymphoma (= malignant Lymphoma) elevated. This is a malignant disease of the Lymphatic system.
prophylaxis
Since celiac disease is an autoimmune disease, prophylaxis is not possible.
-> Continue to the topic of nutrition in celiac disease
Further information
Further interesting information about bowel diseases can be found at:
- Minimally Invasive Surgery
- Gastrointestinal bleeding
- Ulcerative colitis
- Diverticulitis
- Crohn's disease
- Colon cancer
- Stomach cramps after eating
All topics that have been published on the field of internal medicine can be found at:
- Internal medicine A-Z




.jpg)