Cervical Spine Syndrome- How you will be helped!
Synonyms
- Cervical spine syndrome
- Cervical syndrome
- Chronic cervical spine problems
- Neck pain
- Cervicalgia
- Cervicobrachialgia
introduction
More and more people suffer from acute or chronic pain in the cervical spine.
The reasons for this are diverse. One of the main reasons is certainly to be seen in the fact that more and more people today spend a large part of their time sitting. Computer work, frequent television viewing, long car journeys - all of these contribute significantly to the fact that back pain in general, and in particular cervical spine complaints, has increased rapidly in recent years.

causes
In most cases, the causes of a cervical spine syndrome lie in the various components of the musculoskeletal system in the cervical spine. This part of the back is most flexible and therefore also prone to wear and tear on the vertebral body joints and bony attachments on the vertebral body edges.
In younger people in particular, muscle tension in the neck or shoulders is the most common cause of complaints from the complex of the cervical spine syndrome. This in turn can be caused by poor posture, frequent and long sitting, and a lack of physical activity through sport.
Another factor that should not be underestimated in the development of a cervical spine syndrome is stress, which can also trigger or promote muscular tension.
Rarer causes are, for example, inflammatory changes due to an infection or a rheumatic disease.
In addition, a cervical spine syndrome can develop as a result of a previous accident (for example, whiplash after a rear-end collision or sports injuries) or after an operation on the cervical spine. A one-sided posture or movements at work can also lead to the typical symptoms of a cervical spine syndrome, as can incorrect head positioning while sleeping.
A herniated disc in the cervical spine is rarely the cause of a cervical spine syndrome.
Read a lot more information under our topic:
- Causes of a cervical spine syndrome
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Overview of the diseases that can cause a cervical spine syndrome
The following diseases of the cervical spine can lead to a cervical spine syndrome:
- Degenerative spinal diseases
- Spinal canal stenosis (spinal canal stenosis of the cervical spine)
- Facet syndrome
- Osteochondrosis
- Herniated disc of the cervical spine
- Disc protrusion of the cervical spine (protrusion of the cervical spine)
- Blockages (segmental dysfunction)
- Whiplash (cervical spine distortion)
- Muscle tension disorders
- Somatoform pain disorder
- Fibromyalgia
- and much more
Causes due to wear
Wear-related causes of the spine pose a major challenge for everyone involved. The patients have often been plagued by complaints for a long time and thus the muscles have become shorter due to the constant tension. The therapy here is very complex. Therapy begins immediately after the symptoms have subsided. Since the wear and tear cannot be reversed, those affected run the risk of relapse at any time. The aim of the treatments is to strengthen the back, because only strong muscles can stabilize the spine. Active cooperation and initiative can have a very positive effect on the process and result in faster freedom from symptoms.
Herniated disc of the cervical spine
As with the other causes of the cervical spine syndrome, the course of the herniated disc is also very variable. Again, many factors and the extent of the herniated disc play a major role. The chances of success of the therapy are very high, but the course is often protracted, a treatment duration of 3-6 months is realistic. In addition, there have been reports of spontaneous healing of those affected by reducing the herniated disc, on the other hand also cases of permanent damage to nerves or vessels that can no longer be healed and force the patient to undergo lifelong treatments.
Read more on the topic:
- Progress of a herniated disc
Mental causes
Psychological causes can also be treated physically with warmth or physiotherapy. However, the elimination of the emotional causes is extremely important here. People afflicted with stress can use relaxation methods, psychotherapy or methods such as biofeedback to either deal with their complaints or to resolve their internal conflicts. These therapeutic approaches are very long-term and the duration often cannot be estimated in advance. In the case of major psychological problems, depth psychological treatment may often be necessary. This therapy aims to uncover deep conflicts in people, which are physically noticeable here in the cervical spine syndrome. The depth here describes both the depth of the psyche and the depth of time. In the extreme case, unconscious events are processed up to early childhood. This therapy is very protracted, and in the short term it is often not successful.
In summary, it can be seen from the text at the latest that there is no fixed period in which one can be freed from the cervical spine syndrome. Relief from pain is often very quick, and treating the cause can be very tedious. The therapy includes too many components (physiotherapy, drug therapy, heat and cold applications up to psychological therapy) to be able to make an exact statement about the duration. Affected people themselves can, however, have a positive influence on the individual course of the disease by strengthening their backs, solving possible emotional problems and continuously redesigning their habits to be more back-friendly in order to become and remain as symptom-free as possible.
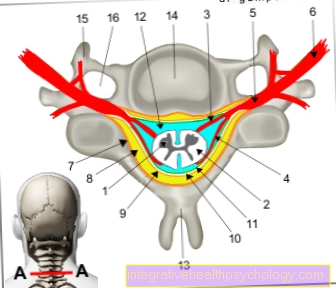
Figure cervical spine syndrome

1st - 3rd - cervical spine (cervical spine)
- First cervical vertebra (carrier) -
Atlas - Second cervical vertebra (turner) -
Axis - Seventh cervical vertebra -
Vertebra prominent - First thoracic vertebra -
Vertebra thoracica I - Shoulder corner - Acromion
- Humerus head - Caput humeri
- Shoulder blade - Scapula
- Humerus - Humerus
- Twelfth thoracic vertebra -
Vertebra thoracica XII - Parietal bone - Parietal bone
- Cerebrum - Telencephalon
- Cerebellum - Cerebellum
A - back of the head
B - neck
C - shoulder
D - upper arm
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms
The term cervical spine syndrome encompasses various unclear pain conditions in the cervical spine. Possible common symptoms of the cervical spine syndrome are, for example, pain in the neck and shoulder area and also neck and back pain, which are mainly caused by tension or hardening of the muscles (muscle tension).
This pain can be burning or pulling and can extend to the inside of the shoulder blades and the back of the head. The pain often increases with head movements. The hardening in the shoulder and neck area can result in a crooked posture, which leads to further tension in the muscles.
Neck stiffness and pain when moving the head can also indicate a cervical spine syndrome. In some cases, headache that spreads from behind the skull (tension headache) can be a symptom of cervical spine syndrome.
The cervical spine syndrome can also temporarily lead to migraine attacks, sleep disorders, relative restlessness and extreme fatigue.
In the early stages of the disease, the symptoms appear only rarely and for a short time, usually they are triggered by certain head movements. In more advanced stages, the pain can also occur at rest and at night and thus become chronic. The affected person is often severely restricted in everyday life by the symptoms of the cervical spine syndrome.
Noises in the ears, dizziness, balance disorders, swallowing difficulties, nausea and visual disturbances are also described. These symptoms often occur in stressful or stressful situations.
If a nerve squeezing or irritation is responsible for the cervical spine syndrome, it can lead to numbness and sensory disturbances (for example "ants tingling" in the arms or head).
Read also: Numbness of the head and scalp
In addition, blockages in the cervical spine syndrome can also affect the autonomic nervous system, which can lead to increased sweating, palpitations and nervousness.
In some cases, in the advanced stage of the cervical spine syndrome, feelings of weakness and a reduction in strength can occur, in extreme cases up to paralysis.
If the cervical spine syndrome is caused by whiplash or a sports injury, there are often no symptoms at first. It can happen that neck and occiput headaches only appear days or months later and the mobility of the cervical spine is increasingly restricted. The stiff neck is often accompanied by severe headaches.
Read more about this:
- Symptoms of cervical spine syndrome
- Shoulder Neck Pain - What You Should Know About It
Concomitant symptoms
Cervical spine syndrome and headache
Headache combined with dizziness is not a rare symptom of cervical spine syndrome. Muscle tension in the neck and shoulder area can lead to severe headaches. The reason for this is often that the muscle tension irritates the meninges, which are very much enervated and react with pain symptoms. On the other hand, headaches with dizziness can also be caused by a circulatory disorder. Even small misalignments and tension in the area of the cervical vertebrae can impair the blood supply to the brain and the sensory organs, which can trigger headaches and even migraines.
The therapy for these symptoms consists of a combination of physiotherapy to loosen and strengthen the neck muscles, as well as massage and medicinal treatment to relieve pain and relax the muscles.
Read more on this topic at:
- Cervical spine syndrome and headache
- Neck pain with headache
Cervical spine syndrome and dizziness
The symptom of dizziness in the cervical spine syndrome is often associated with an unsteady gait or a disturbed feeling of position in space. The dizziness increases with movements or after prolonged tense head posture and often parallel pain in the neck area occurs.
Dizziness caused by cervical spine syndrome can last only a few minutes or stretch for several hours. Certain sensory and nerve cells transmit information from the muscles and tendons in the shoulder and neck area to the balance organs.
With every change in the position or posture of the muscles, the brain can regulate balance and spatial orientation. Tension in the neck muscles, herniated discs in the cervical spine or other triggers of the cervical spine syndrome can interfere with the exchange of information between the sensory cells and the balance organs, causing dizziness.
The diagnosis of vertigo triggered by a cervical spine syndrome is in most cases a diagnosis of exclusion, as many other causes of vertigo symptoms must first be clarified. The treatment of dizziness can be very different depending on the cause; the relaxation of tension in the shoulder and neck muscles usually improves the symptoms of dizziness within a short time.
Anti-inflammatory and pain-relieving medications in conjunction with physical therapy exercises, acupuncture, neural therapy or massages can also improve the dizziness caused by a cervical spine syndrome.
For more information, please also read our topic:
- Cervical spine syndrome and dizziness
Cervical spine syndrome and nausea
The consequences of a cervical spine syndrome can be very complex. Typical complaints are above all sore throats and neck pain, Visual disturbances, Headache and dizziness. Although less often, nausea is also described in some cases. In many cases this is to be assessed as a consequence of the vertigo. Often there is therefore a combination Headache with nausea
Likewise, it is possible that the nausea is a vegetative reaction of the body to the Pain This often occurs with severe or persistent headaches.
Since vertigo symptoms in particular are difficult to treat, therapy for nausea in the cervical spine syndrome starts with one Elimination of pain on. For example, this can be done using Painkillers such as paracetamol or ibuprofen. Weak opioids like tramadol or Tilidine should be used with caution as they run the risk of making the nausea worse. In order to take targeted action against nausea, antiemetics (Nausea medication) like Vomex (Dimenhydrinate) or United States (Alizapride) to disposal.
Cervical spine syndrome and visual impairment
Visual disturbances are pathological changes in optical perception. Visual disturbances can manifest themselves, for example, through flickering eyes, reduced visual acuity, restricted visual field or double vision.
With the cervical spine syndrome, there are sometimes visual disturbances in combination with a migraine attack. In addition to severe headaches, flashes of light or flickering eyes can occur.
The visual disturbances that occur in a cervical spine syndrome are mostly caused by circulatory disorders in the brain, for example triggered by a narrowing of an artery in the cervical vertebrae. Two small vertebral arteries run right and left through a bony canal in the cervical spine and supply the brain with oxygenated blood. In the case of a cervical spine syndrome with a narrowing of one of the two arteries, particularly with extreme head rotations, circulatory disorders and thus an insufficient supply of the brain can occur, which triggers the visual disturbances.
A herniated disc in the cervical spine can cause visual disturbances in addition to many different symptoms (such as paralysis of the arms, numbness or tingling). In general, visual disturbances in the cervical spine syndrome are a rather rare symptom and occur in particular in psychological stressful situations.
Read more on the subject:
- Cervical spine syndrome and visual impairment
- Eye flicker
difficulties swallowing
Difficulty swallowing can be a symptom of the cervical spine syndrome. Therefore, if you have difficulty swallowing, you should always rule out a problem with the cervical spine.
On the one hand, a smooth act of swallowing requires a functioning skeleton so that, for example, the jawbone can move freely. If the cervical spine is changed due to an accident, bad posture or wear and tear (degeneration), the position of the jaw and the temporomandibular joint can also be changed, which makes the act of swallowing difficult or even painful.
Furthermore, in the context of a cervical spine syndrome, osteophytes can arise from the cervical spine and cause swallowing problems. These increases in the vertebral bodies can mechanically constrict the esophagus.
In addition, due to inflammatory processes in the cervical spine, swelling of the surrounding tissue can lead to mechanical restrictions when swallowing. Sometimes these runners are perceived by the patient as a foreign body sensation.
Another possibility for swallowing difficulties in combination with sudden neck pain and stiff neck could be tendon calcification of the muscle directly in front of the cervical spine (M. longus colli). This tendon calcification can occur in the course of a cervical spine syndrome. The calcification of the tendon is accompanied by an inflammatory process. This inflammation can spread to the throat muscles, which are very important for the swallowing process.
This can cause muscle spasms and pain in the throat while swallowing.
Cervical spine syndrome and muscle hardening
The list of symptoms that can be triggered by the cervical spine syndrome is quite long. Besides sore throat and neck pain, dizziness and headache are also the so-called Myogelosis very typical symptoms of cervical syndrome. This is a circumscribed hardening of the muscles. Common slang terms are Hard clamping or Callosity. They express themselves as painful on pressure, olive-sized, running along the fiber direction of the muscle Indurations and are mostly found on heavily stressed muscle areas, such as the straight back muscles. Due to the pain caused by the cervical spine syndrome, patients often take unnatural ones Relief postures of the shoulder girdle and the cervical spine area. In response to this Improper loading myogeloses can also form here. They are usually treated first with massages and physiotherapy exercises. In addition, or if the therapy is unsuccessful, you can also Painkiller or Muscle relaxants (Medicines to relax the muscles) can be used. One is also helpful Heat therapy with red light or warm pillows and compresses.
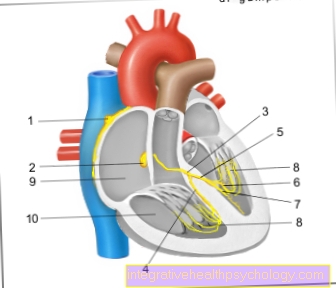
Cervical spine syndrome and high blood pressure
The phenomenon that the Blood pressure drops when a chiropractor flexes a cervical vertebra has long been known. However, it took a while to figure out how to do it high blood pressure (hypertension) at a Cervical spine syndrome can come. In the meantime it has been found that the neck muscles are connected to a brain area, which is a Control function on blood pressure, breathing and heartbeat exercises. For example, tension in the shoulder and neck muscles in the case of a cervical spine syndrome can send unusual signals to this area of the brain, thereby influencing blood pressure.
The neck muscles play an important role in assessing the position of the body in space. Even small changes in posture are passed on to the brain by the neck muscles. If there is a cervical spine syndrome, the communication between the brain and neck muscles is disturbed, and incorrect information is passed on. For this reason, symptoms and complaints such as cervical spine syndrome may occur dizziness, Headache and just high blood pressure. In addition, a chronic pain burden on the neck muscles leads to the cervical spine syndrome increased stress for the whole body. In humans, stress manifests itself through restlessness, sleep disorders, sweating and also through an increase in blood pressure. In many cases, treating the cause of the cervical spine syndrome can normalize blood pressure without having to take antihypertensive drugs. Often the treatment of the cervical spine syndrome alone leads to pain-relieving, anti-inflammatory and tension-relieving drugs physiotherapy Exercises, Massages or Heat therapy to an improvement in the symptoms of high blood pressure.
Since high blood pressure can have numerous causes, one should definitely be thorough examination of a doctor respectively. In most cases (around 95%), high blood pressure is what is known as essential hypertensionwhich means that in these cases no direct cause of the high blood pressure can be identified.
Cervical spine syndrome and heart problems
A wide variety of symptoms can be associated with a cervical spine syndrome. These mainly include headaches and neck pain, as well as dizziness, ringing in the ears, and numbness in the upper extremities.
Symptoms of other organ systems are also often assigned to the cervical spine syndrome. In addition to the lungs and the digestive organs, this also includes the heart. Although no specialist literature or current studies are available, a connection between symptoms of the heart, such as palpitations (extrasystole), and a cervical spine syndrome is not absurd. The nerve fibers of the autonomic nervous system, consisting of the sympathetic and parasympathetic parts, run along the spine. This system controls body functions such as blood flow, gastrointestinal peristalsis, breathing and also the heart function - independently of conscious influencing.
The nerve responsible for supplying most of the internal organs (vagus nerve) runs through an opening in the skull on both sides along the carotid arteries and later down the esophagus towards the chest. It is entirely conceivable that chronic tension in the neck muscles can lead to irritation of the vagus nerve and, as a result, to cardiac stumbling every now and then.
The sympathetic nerves, the second part of the autonomic nervous system, also run close to the spine. The nerves that control the heart function collect in the area of the cervical spine to form a network of nerves and can therefore be irritated or injured in the course of a cervical spine syndrome due to misalignments and blockages of the cervical vertebrae or an intervertebral disc prolapse of one or more cervical vertebrae. As a result, the sympathetic control can get mixed up in a cervical spine syndrome. The sympathetic nervous system normally ensures that the heart beats faster and more vigorously, for example under stress. If injuries to the cervical spine irritate these nerves, it can cause the nerves leading to the heart to give false signals. This can lead to palpitations, palpitations or arrhythmias.
Recurring heart problems are to be treated primarily by treating the cause, in this case the cervical spine syndrome.
Read more on the topic:
- Stumbling heart through back (pain)
Deaf fingers
With cervical spine syndrome, some people occasionally have numb fingers as an added symptom.
Both or just one hand can be affected. In addition, not all fingers of a hand are usually affected to the same extent. The cause of the symptom is that in the cervical spine syndrome the nerve roots emerging from the spinal cord in the cervical spine can be irritated. Many of these nerve pathways run to the arms and ultimately to the fingertips. Among other things, they convey sensations from the fingers back via the spinal cord to the brain, where they are perceived. Irritation in this way can cause discomfort such as numb fingers.
However, since another cause such as a herniated disc or a pinched nerve in the hand can be responsible for these symptoms, a medical examination should be carried out in case of doubt.
You may also be interested in this topic:
- Carpal tunnel syndrome
Cervical spine syndrome and the psyche
The cervical spine syndrome, like many other chronic diseases, is in many ways related to the psyche. Many patients who suffer from a chronic illness are diagnosed by a doctor as having a psychological cause for their symptoms. This is mainly due to the fact that a physical cause of the cervical spine syndrome is often difficult or difficult to determine and a wide variety of treatment methods are inadequate. This is associated with great frustration both for the attending physician and, above all, for the patients, as they feel they are not being taken seriously. Nevertheless, the cervical spine syndrome can actually also have a psychosomatic background. Our (often unconscious) mental state often has a greater impact on our physical well-being than we'd like to admit. A psychologically stressful stressful situation of any kind can lead to tension in the neck and neck area, which in turn triggers the symptoms typical of the cervical spine syndrome.
You can read more about this under:
- Cervical Spine Syndrome - Effects and Consequences
Duration
How long the symptoms last in a cervical spine syndrome depends entirely on the cause and the extent of the disease. Basically, it is important to recognize the trigger of the cervical spine syndrome at an early stage and to initiate an individually appropriate therapy. In order to prevent long-term discomfort caused by a cervical spine syndrome, posture correction should be carried out through physiotherapy exercises, the cervical spine should be stabilized through muscle building, incorrect loads during sport should be avoided and ergonomic aspects should be observed in everyday work.
If the pain persists without a previous accident, a doctor should be consulted after one to two weeks at the latest. On the other hand, an immediate visit to the doctor is indicated in the event of persistent sensory disturbances in the shoulder or arm, dizziness, ringing in the ears, paralysis, visual disturbances or after an accident. If the cervical spine syndrome is left untreated for a few years, the permanently increased muscle tension can shift the position of the cervical vertebrae in relation to one another. This leads to greater stress and wear and tear on the cervical spine, which is reflected in a narrowing of the disc space. Acquired spinal misalignments can hardly be normalized, but in most cases the symptoms can be alleviated.
If the symptoms improve within 3 weeks, one speaks of an acute (= sudden) cervical spine syndrome. If the symptoms last longer than 3 months, one speaks of chronic (= persistent) cervical spine syndrome. In between there is a kind of transition period between the forms, which is then referred to as "subchronic". As a rule of thumb, the longer the symptoms exist, the longer the treatment will take. During this time, however, those affected do not have to continue to suffer from their mostly not inconsiderable symptoms. From the very beginning, painkillers can and should be prescribed by the doctor so that those affected are pain-free quickly and therapy can then be started. Medicines that relax the muscles also provide additional rapid relief. However, both drugs are not suitable for combating the causes and must also be treated intensively.
In summary, the following applies: the time until pain is free should be relatively short, the time until the cause is improved is significantly longer.
The cause of a sudden (= acute) cervical spine syndrome is what is known as "whiplash". Rapid braking in traffic accidents leads to massive overstretching of the head, including all structures in the cervical vertebra area. The massive stretching can lead to injuries to structures in this space. These then cause the patient the typical complaints such as neck pain or neck stiffness, since the neck muscles react to such massive stimuli with complete tension. The healing of this damage determines the duration of the complaints. In many cases, the injuries heal within days to weeks without any consequential damage. However, whiplash can also turn into a persistent cervical spine syndrome with permanent symptoms. This must be avoided. Previous damage to the cervical spine can also delay the healing process. Physiotherapy exercises, on the other hand, can shorten the days until recovery.
If blockages of the cervical spine (= smallest vertebral displacements) are the cause of the cervical spine syndrome, even a few physiotherapeutic treatments can bring an extreme improvement in the symptoms. The slightest shift leads to an imbalance in the sensitive system of bones, muscles and ligaments that hold the spine in its plumb. You can see these effects most impressively in the massive tension in the neck muscles. In addition, these shifts can also press on nerves, which has effects in the form of tingling, numbness, pain, etc. on various parts of the body. If the cause is now brought back into balance by an experienced therapist or doctor with the help of special techniques, an immediate improvement often occurs. The diagnosis of a cervical blockade is usually preceded by a long medical history. Success can be achieved through several treatments of different nature (e.g. warmth to loosen up the muscles plus physiotherapy). This can also accelerate the improvement of the condition. Here, too, the longer the symptoms have persisted, the greater the changes in the muscles and ligaments and the longer it can take to bring them back to an almost improved state.
Read more on the topic:
- Duration of a cervical spine syndrome
therapy
The treatment of the cervical spine syndrome is primarily intended to loosen the tense shoulder and neck muscles in order to eliminate the pain. Depending on the severity and extent of the symptoms caused by the cervical spine syndrome, the most suitable therapy option can be selected. This should be done in consultation with the treating doctor or therapist.
For pain therapy, anti-inflammatory and pain-relieving medications can be used, as well as muscle relaxants to relieve the tense shoulder and neck muscles.
The so-called wheal therapy has a pain-relieving effect and relaxes the muscles. A medication (e.g. a local anesthetic) is injected under the skin at the painful area.
Local heat applications have a similar effect, as the muscles are relaxed and tensions are released. For example, warming plasters, creams and the like are suitable for this.
The therapeutic use of baths (balneotherapy) can also provide relief.
A manual massage can also alleviate the symptoms of the cervical spine syndrome. Massages are often combined with heat treatments such as red light irradiation or heat packs.
However, if the cervical spine syndrome recurs, massages are common unsatisfactory, under physiotherapeutic guidance with specific exercises, the blood circulation in the shoulder and neck area should be improved, tensions removed and the muscles strengthened.
The so-called iontophoresis (stimulation current treatment) offers a therapy option for the cervical spine syndrome. Iontophoresis uses an electric current to introduce small amounts of muscle-loosening drugs into the subcutaneous tissue. This electrical stimulation treatment takes about ten to twenty minutes and requires more repetitions to achieve a sufficient effect (at least six applications). Electro-stimulation treatment is not indicated for people with pacemakers or metal implants.
Ultrasound treatment is another therapeutic method against the symptoms of the cervical spine syndrome. An ultrasound head, from which inaudible sound waves emanate, is moved by a therapist over the tense muscles. These sound waves cause internal friction in the tissue and generate heat. This creates a so-called micromassage that relaxes tension.
The long-term success of therapy for the cervical spine syndrome depends above all on the person affected learning how to avoid renewed overload and finding a suitable exercise that alleviates the symptoms.
Further information can also be found here:
- Neck Syndrome Exercises
- How can you best relieve neck tension?
physical therapy
The tasks and possibilities of physiotherapy (physiotherapy) essentially cover three aspects in the treatment of acute or chronic complaints of the cervical spine:
- Pain relief and control of the disturbed muscle tension state (muscle tone).
- Stabilization and targeted muscle building of the supporting muscles in the cervical spine.
- Recognizing and switching off the triggering factors (prophylaxis)
1. Pain relief and regulation of the disturbed muscle tone (state of tension):
This topic is certainly the most important in the first, acute phase of the complaint. The main concern in this early phase of the cervical spine syndrome is to combat the pain problem. In the following, only the physiotherapeutic therapy options are discussed. For treatment options within the range of medical therapies, reference is made to the individual clinical pictures.
Often the cause of the complaints is an increase in pressure on the intervertebral discs, especially the lower cervical vertebrae. This can also lead to pressure on the paired nerve roots in the intervertebral hole (neuroforamen) going off between two vertebrae.
Therefore, a promising therapeutic method is the manual relief of the intervertebral discs and nerve roots by carefully pulling in the longitudinal direction of the head (traction).
Another tried and tested option for treating pain is to relax tense muscles using targeted massage techniques. The focus here is primarily on the shoulder-neck massage, which is extremely tense in almost all patients with problems of the cervical spine. Stretching, also known as stretching, of the affected muscle fibers has a similar effect. Stretching by an experienced physiotherapist is certainly more effective, but you can also achieve good results through self-stretching.
One type of therapy that is often used in manual therapy and also in traditional Chinese medicine (TCM) is “trigger point treatment”. Characteristic pain points are treated with pressure treatment.
In the acute phase of the symptoms, it is often advisable to supplement the physiotherapeutic measures with local application of heat (e.g. fango, red light, etc.). Muscle relaxation caused by warmth often already relieves pain. The maximum relaxing effect can be achieved if a relaxation massage follows after the application of heat, since the tense muscles are already in a relaxed state and are more accessible for therapy.
2. Stabilization and targeted development of the supporting muscles in the cervical spine:
In the case of the cervical spine syndrome, this part of physiotherapy usually only starts when the acute pain has already subsided somewhat. An effective muscular exercise program can strengthen the weakened muscle groups and thus prevent the symptoms from occurring again, or at least significantly reduce the intensity of the pain. Strengthened muscles tire less quickly, are thus overloaded less quickly and thus offer better and longer protection for the non-trainable structures of the cervical spine (intervertebral discs, vertebral joints, etc.)
First of all, an isometric strengthening of the muscles should take place. In this context, isometry is understood to be a muscle tension, in which, however, there must be no visible movement. The origin and insertion of the muscles do not converge. The patient is only exposed to such a great resistance that he can respond painlessly with his individual performance.
The proper integration of the cervical spine into the upright posture should also be worked out in this therapy phase at the latest. Axial integration in this case means that the head is held straight as an extension of the spine. An important principle in strengthening training in all areas of the spine is based on the fact that the back is stabilized, i.e. it does a purely holding work and does not perform any active movement. The training effect for the back sets in because active movement exercises of the arms make it even more difficult to hold the core muscles.
With all complaints of the cervical spine, it should also be remembered that the cause of the complaint may well be in other parts of the body. Whenever neck pain occurs, the shoulder region should also be examined. The thoracic and lumbar spine (thoracic spine, cervical spine) must also be examined regularly. Quite a few pain problems in the cervical spine are actually caused by a disruption of the underlying spinal column.
3. Recognizing and eliminating the triggering factors:
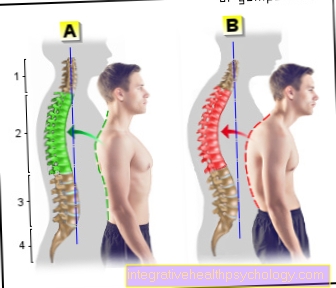
The third point in the physiotherapeutic treatment of cervical spine syndromes, which is decisive for the long-term therapeutic effect, is the elimination of the causative disorders (prophylaxis). This includes, for example, learning back-friendly everyday behavior and avoiding particularly stressful movements. This can be illustrated particularly well using the example of the sitting posture at the computer.
After long periods of sitting, most people adopt an increasingly "crooked" posture. Often the shoulders are then pulled up when typing on the keyboard, which leads to the typical tension in the shoulder and neck muscles in almost all patients working at their desks. In order to still have a good view of the screen, the cervical spine is often overstretched, which increases the pain problem or can lead to further complaints. A physiotherapeutic treatment of the resulting cervical spine syndrome that promises long-term success can only take place if such misconduct is avoided. To do this, it is necessary to identify and eliminate such misconduct.
Even minor changes in the work environment or in everyday life often bring about significant relief from the symptoms. For example, the unfavorable positioning of the monitor when working on the computer alone can be the main cause of painful tension in the neck and neck muscles. Fortunately, things have changed for the better in this area in recent years. Many companies are trying to make working conditions as back-friendly as possible. The keyword “workplace ergonomics” is becoming more and more important in avoiding chronic back pain (back-friendly everyday behavior / neck school). Company doctors help set up an ergonomic workplace in many companies.
Read more on this topic at:
- Physiotherapy for a cervical spine syndrome
Osteopathy
Osteopathy is a treatment method that can be assigned to alternative medicine. The philosophy of Ostheopathy says that the person is treated in his entirety and underlying disorders of ailments are treated so that a natural energetic and functional harmony is restored.
In an osteopathic treatment of a cervical spine syndrome, the body and head posture of the person concerned is first assessed while standing and sitting. The tension of the connective tissue is tested over the entire surface of the body and the tense muscles felt. The restriction of movement caused by the cervical spine syndrome is checked in a side-by-side comparison.
The osteopathy therapy then consists of a combination of head rotations, muscle tension by the person affected and precisely defined movements of the cervical spine by the osteopath.
As a rule, each vertebra is treated individually and adjacent joints such as the shoulder are examined and treated for restricted mobility. After the bony blockages have been resolved, the osteopathic treatment involves loosening the adjacent soft tissues, muscles, ligaments and connective tissue.
Read more on this topic at:
- Osteopathy in cervical spine syndrome
Homeopathy for cervical spine syndrome
Treatment of the cervical spine syndrome is often very tedious and only provides unsatisfactory results. For this reason, many patients resort to naturopathic alternatives after failed attempts at conventional medicine. First of all, on the subject of homeopathy for cervical spine syndrome, it should be mentioned that there are no meaningful studies on the effects of homeopathic remedies in general. The theoretical foundations of homeopathy (such as the principle of potentiation) even contradict current chemical and physical knowledge. At the same time, the homeopathic remedies offered are not regulated by the currently applicable Medicines Act, but are subject to their own, scientifically unjustifiable regulations.
Nevertheless, a number of different homeopathic remedies are available for treating the cervical spine syndrome. Depending on the cause, quality and location of the pain or tension caused by the cervical spine syndrome, preparations such as Rhus toxicodendron, Actaea racemosa, Arnica or Bryonia are used. More detailed information on this can be obtained from an appropriately trained alternative practitioner.
However, caution is required in any case should the pain intensify or widen acutely. In this case, it is always advisable to seek medical advice.
Also read: Homeopathy for cervical spine syndrome
Home remedies
Various simple home remedies have been tried and tested to relieve symptoms caused by a cervical spine syndrome.
Many aim to heat treatment of the affected region in different ways in order to relieve muscle tension. When showering, for example, warm water with a medium jet of warm water can be aimed specifically at the neck for about five minutes. Red light irradiation up to three times a day for about ten minutes each time is also suitable.
Other simple but effective home remedies are movement exercises that should be performed regularly and that do not require any additional aids. In the so-called mill circle, the outstretched arms are moved in opposite directions in wide circles while standing and guided close to the body. The direction should be changed occasionally.
Exercise for a cervical spine syndrome
Strong and relaxed back and neck muscles form the basis for completely healing a cervical spine syndrome and preventing it from developing again. Therefore, physical activity and exercise are expressly recommended in the cervical spine syndrome.
However, if you have problems with your spine, you must choose sport well, as sport that is too strenuous or stressful for your spine can otherwise trigger a cervical spine syndrome. Breaststroke swimming, for example, should be avoided, as this can quickly tense the neck muscles and cause problems in the cervical spine. A suitable type of swimming is backstroke swimming. The back and the spine in general are strengthened and the neck is relieved.
In addition, water sports do not damage the spinal joints as can be the case, for example, when jogging. Yoga is also very suitable for strengthening the back muscles. Yoga also helps to reduce emotional stress, which can also trigger tension in the neck and back. Other suitable sports are, for example, hiking and walking, but also gentle strength training. In any case, the physical activity should always be adapted to the individual fitness level.
You can find more information on this topic at: Exercises in cervical spine syndrome
Tips for at home
When it comes to self-treatment of the cervical spine syndrome, the symptoms and the respective phase of the complaint are the decisive criteria for treatment.
First, a few words about the possibilities of pain relief during the acute phase. It should be borne in mind that the perception of pain is different for each person. What already means unbearable pain for one, can still tolerate the other relatively well. Accordingly, the following advice and the resulting results are of course perceived differently by individual patients. A “panacea” is not to be expected either, since not every form of treatment is equally effective for all people. The common advantage of all physical and physiotherapy therapies is the good tolerance of the forms of treatment that are used. Unwanted side effects are almost zero.
Thermal (heat / cold therapy) applications represent an important group of physiotherapeutic treatment measures for cervical spine syndrome.
In contrast to cold therapy, heat applications (thermotherapy) are used far more frequently in the cervical spine syndrome. This is a form of therapy that is very effective and suitable for self-therapy at home.
The possibilities at home are, for example, the use of various grain pillows (spelled pillows, cherry stone pillows, etc.), which are heated in the microwave and then placed on the painful areas. Anyone who has a red light lamp can also use it well.
Less known, but very effective heat applications are the so-called "hot role". First, hot water is poured into a funnel-shaped rolled towel. Then dab the painful areas of the body with the wet towel. The advantage over a grain pillow or a hot water bottle is that this moist warmth promises greater healing success.
The second somewhat forgotten possibility of heat therapy is to make a compress from boiled jacket potatoes. The boiled potatoes are mashed a little and placed in a cloth, which must not be too thick, so that enough heat comes through (e.g. tea towel, linen cloth) This cloth is then placed on the painful areas of the body and left there for some time. The starch contained in the potatoes removes the resulting metabolic “waste” from the muscles. The duration and frequency of the different heat applications depends entirely on personal feelings. In principle, there is nothing to be said against daily heat therapy.
The possible uses of cold therapy (cryotherapy) are rather limited in the cervical spine syndrome. Only in a few exceptional cases does it have authorization, e.g. in an inflammatory overheating of the muscles. In this case, the muscles should be cooled, but I would like to expressly and fundamentally recommend a "gentle" method. I strongly advise against using ice or even using ice spray. Sub-zero temperatures are actually no longer used in modern physiotherapy. One possibility of sensible application of cold would be, for example, therapy with cold, damp cloths.
Quark packs have been a tried and tested home remedy for years and are a good way of lowering overheated muscles to a physiological (normal) temperature. Commercial quark is applied to the inflamed area and covered with a cloth. After about 15-20 minutes, the quark is simply removed again.
In the case of strong tension in the neck muscles, it is worth trying to achieve relaxation with a self-exercise based on the principle of pressure point treatment. This treatment is not exactly pleasant at first, but it is extremely effective for certain causes of pain (e.g. painful muscle swelling). Tennis balls that are first placed on the floor are suitable for self-treatment. Now you lie on your back on the ground and lie down with your tense muscles directly on the tennis balls. This pressure is quite painful and uncomfortable at first, but after a while the discomfort subsides and the muscles begin to relax.
Medication
Purely physiotherapeutic and physical therapy may not be sufficient, especially in acute phases of pain. Here, the use of additional drug therapy is required. This should always be discussed with your treating doctor! In this way, undesirable side effects and complications can be minimized and any intolerance / contraindications discussed.
In the case of a cervical spine syndrome, drugs are often used for short-term treatment. In most cases, pain reliever and anti-inflammatory tablets are prescribed. By relieving symptoms, these should help to ensure that natural activity and movement are possible in order to release the usually underlying muscular tension.
On the other hand, pain medication is not suitable for long-term use as long-term therapy due to dangerous side effects over a period of time longer than a few days. Some doctors also prescribe muscle relaxant drugs directly, although their use in cervical spine syndrome is controversial. The same applies to injecting drugs such as local anesthetics directly into the muscles in the neck or at the nerve exit points. Most doctors today advise against such procedures because the effect is only short-term and the treatment is associated with risks such as the risk of inflammation. Long-term relief from a cervical spine syndrome should not be achieved through medication, but through sufficient healthy exercise and occasional heat applications.
Drugs suitable for treating cervical spine syndrome are:
- NSAIDs
- Ibuprofen
- Diclofenac
- Celebrex
- Paracetamol
- Novalmine sulfone
- Tramadol
- Valoron
- Katadolon
- Devil's claw
- and much more
Have a muscle-relaxing effect:
- Mydocalm
- Diazepam
diagnosis
The cervical spine syndrome describes an inconsistent combination of different symptoms that can be caused by very different clinical pictures. Therefore, there is no examination by which the diagnosis can be made.
Rather, when making the diagnosis, it is initially excluded that there is another specific clinical picture. If there is no evidence of this, the diagnosis of cervical spine syndrome can be made in the case of uncharacteristic complaints in the neck, cervical spine and shoulder region. When presenting to the doctor, the first steps are therefore the most important for the further procedure. On the one hand, in the medical interview (anamnesis) it is asked exactly which symptoms have been present, since when they have existed, which triggers them and if necessary alleviates them.
In addition, a targeted physical examination takes place, during which the doctor pays attention to possible misalignments, tension and inflammatory reactions. Depending on the findings from the anamnesis and the physical examinations, the doctor will decide whether further diagnostics are indicated for clarification or to rule out other causes, or whether the diagnosis of a cervical spine syndrome can be made. It is important to inform the doctor about your own ideas or concerns about the symptoms you have experienced.
MRI
An MRI (magnetic resonance tomography) should not be used regularly in the diagnosis of a cervical spine syndrome. A cervical spine syndrome can be diagnosed if there is no evidence of a serious cause of the symptoms or causes of the symptoms that require specific treatment. In such a case, an MRI would usually not show any abnormal findings.
An MRI should only be used if this complex diagnosis is associated with a consequence for the treatment of the patient. This can be the case, for example, if the doctor suspects on the basis of a conspicuous finding in the physical examination that there is a pronounced herniated disc that may have to be operated on or if an injury in the cervical spine has to be ruled out due to an accident. Often, however, a simple X-ray or computed tomography (CT) is performed first.
- MRI of the cervical spine