Heart failure therapy
How is the treatment of cardiac insufficiency carried out?
The therapy of the Heart failure sometimes too Heart failure called, is divided into general measures to improve the quality of life, dietary measures and the administration of various Medication (possibly a combination therapy depending on the stage).
General measures include regular physical activity that is individually tailored to the patient's capabilities.
This has been shown to improve the damage to the vascular walls caused by heart failure / cardiac insufficiency (medical: Endothelial dysfunction).
The goal of dietary measures is in the presence of Obesity (obesity) in the reduction of the Overweight (Obesity).
It also contributes to a low-salt diet, varied and reduced hydration diet to prevent Edema and to relieve the heart.
It also has a varied, plenty of fresh vegetables and fruits nutrition favorable to the course of the disease. Especially with existing Cardiomyopathy (medical definition: any diseases of the heart muscle associated with a dysfunction) is abstinence from nicotine (= smoking ban!) and alcohol important.
Another important part of the Therapy for heart failure is the administration of drugs, whereby one can choose from five different drug groups:
- These are so-called. ACE inhibitors (inhibit the formation of heart failure / heart failure promoting messenger substances and relieve the heart by lowering the blood pressure)
- Aldosterone antagonists, Angiotensin 1 antagonists (inhibit the formation of the particular messenger substance that activates the sympathetic nervous system and is responsible for the connective tissue remodeling of the heart muscle cells Angiotensin 2 via so-called angiotensin 1 receptors - here the naming of the pharmacologists is admittedly a little awkward!)
- Beta blockers (which inhibitors of the beta-adrenoceptor receptors of the Sympathetic represent and that heart by preventing the effects of the sympathetic hormones that drive the heart)
- such as Diuretics (whose diuretic effect is used to excrete excess tissue water and which thus reduce the stress on the heart by reducing the total volume to be pumped.
More precisely, ACE inhibitors such as captopril, enalapril and ramipril are the standard drugs in the treatment of cardiac insufficiency and can be given in all stages (according to NYHA, see above).
The mechanism of action consists in the inhibition of the angiotensin conversion enzyme (ACE for short), which ensures the formation of angiotensin II from its ineffective precursor angiotensin I.
ACE inhibitors thus work by reducing all the effects of angiotensin II: The blood pressure-increasing constriction (narrowing) of arterial vessels is reduced, fewer sympathetic messenger substances are released into the blood (angiotensin II causes the release of noradrenaline from peripheral nerve endings and of adrenaline from the Adrenal medulla), the growth-promoting effect of angiotensin II, which is responsible for excessive growth of the heart muscle cells, is abolished and the release of the messenger substance aldosterone, which is responsible for fluid retention in the kidney and thus stresses the heart, is inhibited.
Because the activation of the sympathetic nervous system is reduced, the resistance in the arterial vessels (medical: TPR, total peripheral resistance), against which the left heart has to work when ejecting blood into the body's circulation, decreases.
(To put it medically: the afterload of the heart is reduced. The reduction in the total volume of fluid also contributes to this.
The reduction (diminution) in the volume of blood to be expelled into the systemic circulation, i.e. the reduction in the pre-filling of the heart chambers is analogously referred to as lowering the preload.)
ACE inhibitors are therefore very effective drugs for the treatment of heart failure / heart failure.
However, it should be noted that the apparent miracle drug ACE inhibitors can also cause undesired ACE inhibitor side effects, which make it necessary to switch to another preparation in up to 10% of patients treated with this drug (up to 10% do not Threatening, dry cough; the ACE inhibitors are discontinued, since the angioneurotic edema, which leads to a shock-like condition, can then occur in 0.5% of those treated, which is rare but dangerous.
Very rarely, short-term fainting spells, i.e. a syncope, come.)
Angiotensin 2 antagonists such as candesartan and telmisartan, which have significantly fewer side effects with a comparable effect profile, are therefore an alternative.
Read everything about ACE inhibitors in our topic: ACE inhibitors
Beta blockers - examples of which are metoprolol, bisoprolol and carvedilol - have shown the greatest effectiveness in clinical studies in terms of a life-prolonging effect in patients.
Therefore, the beta blockers are often combined with the ACE inhibitors in therapy.
One mechanism of action is the reduction in heart rate, which is generated by the beta receptors of the heart (Sinus node) is increased; A second mechanism of action, as with the ACE inhibitors, is the inhibition of the formation of the messenger substance angiotensin II, because the beta receptors also occur in the kidneys and there inhibit the release of renin (the starting substance of angiotensin II).
When administering beta-blockers, it is important to monitor the patient closely, since cardiac function can deteriorate, especially at the beginning of therapy, but these drugs are generally well tolerated.
Beta blockers may not be given if:
- asthma
- Circulatory disorders
- or an atrioventricular block of a higher degree (medical: atrioventricular block, this is a disruption of the transmission of electrical excitation from the atria to the ventricles).
For more information, see AV block.
exist.
In the case of very severe cardiac insufficiency in the end-stage ("terminal heart failure"), the salt and fluid intake can be optimally monitored during inpatient therapy. Emergency medication is medication to increase the contraction force of the heart (medical: positive inotropic substances); the most commonly used are dobutamine, which stimulates sympathetic receptors (medically: it's a beta agonist) acts on the heart muscle, as well as levosimendan, which increases the sensitivity of the heart muscle cells to calcium (calcium is needed for every muscle contraction because it is responsible for activating the contractile muscle proteins;
For those interested: By changing the conformation of troponin C, calcium ensures that myosin filaments release the binding sites on actin filaments). You can find more information about the function of the muscles under our topic: Muscles
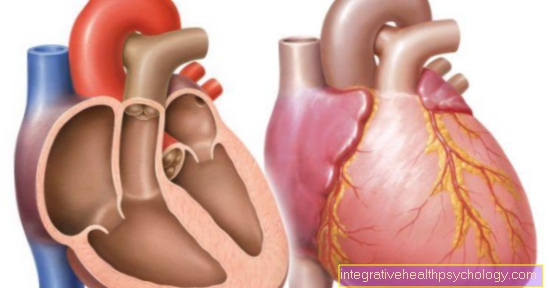
If strict selection criteria are met, the transplantation of a donor heart can be considered as the last resort in the treatment of heart failure.
The prerequisite is the presence of heart failure / heart failure at least stage 3 according to NYHA, that all other, conventional therapy options have been exhausted, and that you are under 60 years of age.
Studies of the last ten years show a clear improvement in the average survival rate (around 70% survive the next five years), but this is offset by strong immunosuppressive therapy after the operation and the need for complex diagnostics before the operation.
In view of the clear influence of previous damage to the heart on the risk of later developing heart failure / cardiac insufficiency, therapy for the classic risk factors that damage the heart (high blood pressure, increased cholesterol levels in the blood) is of great importance.
Please refer to the next article for helpful information on this topic: Heart tablets
diagnosis
Both externally detectable changes as well as physical, technical and laboratory tests are groundbreaking for the doctor.
Indications of an existing heart failure / weakness of the heart are breathing difficulties (tachypnea: accelerated breathing), edema, bluish discolouration caused by a lack of oxygen, e.g. the lips or the end members of the extremities (acra) and congested neck veins.
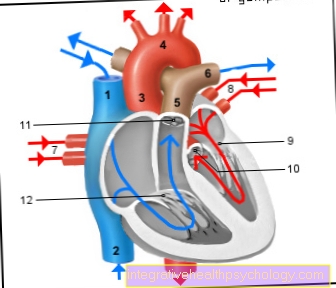
Auscultation performed as part of the physical examination, i.e. Listening to the heart with a stethoscope characteristically often shows the appearance of an additional, third heart sound (normal are a first heart sound that occurs before the contraction of the heart muscle and a second one that shows the closure of the aortic valve and pulmonary valve (both heart valves), so that the two heart tones mark the beginning and end of a heart muscle contraction).
Both a too fast heartbeat (tachycardia) and too slow a heartbeat (bradycardia) can be present. In patients with severe cardiac insufficiency / cardiac insufficiency, the pulse is either accelerated or slowed down in rapid succession (medical: pulsus alternans).
The most important device-based examinations are an ultrasound image of the heart (an echocardiography), an X-ray image of the chest, and an electrocardiogram (EKG for short) made under physical stress.
A simple EKG is less suitable for the unambiguous determination of cardiac insufficiency / cardiac weakness, since the findings that can be determined there could be caused by a large number of diseases and are therefore too unspecific. The ultrasound image, on the other hand, enables a precise representation of blood flow, wall movements of the heart and heart valves; The chest x-ray is used to assess the size of the heart (the heart is often greatly enlarged as an expression of the attempt to compensate for increased stress through increased growth;
So basically the same thing happens as with an athlete training his biceps to build muscle). In the laboratory examination, blood and urine are examined, whereby there are no 100% conclusive changes.
Read more on the subject at: These tests are done if you have heart failure
The messenger substances "ANP" and "BNP" (abbreviations for "Atrial Natriuretic Peptide" or "Brain Natriuretic Peptide", i.e. not always routinely determined in the clinic) provide a strong indication of the presence of heart failure / heart failure.Protein components that are increasingly formed and released into the blood in heart failure / heart failure).
Read more on the topic: Heart failure on the EKG such as Life expectancy with heart failure