Hyperventilation (psychogenic)
definition
The term Hyperventilation stands for the unphysiological phenomenon of accelerated and deepened breathing (hyper = too much, ventilation = ventilation of the lungs).
Physiological regulation
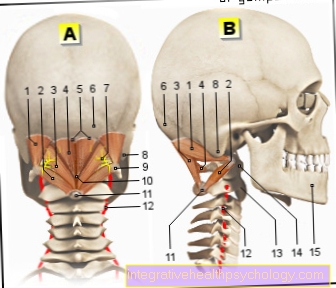
Usually ours will Respiratory drive over neurogenic and chemical stimuli regulated. The chemical stimulus in particular is crucial for hyperventilation. To understand hyperventilation, it is important to understand the physiological chemical respiratory drive. The three main influencing factors are one increased carbon dioxide partial pressure (pCO2), the Increase in protons (H +) and a decreased oxygen partial pressure (pO2).
The strongest respiratory stimulus is set by a drop in pCO2 and is also known as hypercapnic respiratory stimulation. The value is measured by central chemoreceptors in the central nervous system. If the value rises, the body's regulatory mechanisms intervene and stimulate breathing to breathe out the excess CO2.
Furthermore, there is hyperventilation increased depth of breathas the H + number increases. The However, the respiratory rate remains unchanged or increases if necessary. The increase in the H + number makes the blood "acidic" and the pH value sinks below its optimal value of 7.4. The increased exhalation of CO2 goes hand in hand with the decrease in the number of protons, so that the pH value rises again.
The last regulatory mechanism is the over peripheral chemoreceptors, which the pO2 in the blood of aorta and the Carotid body measure up. The condition of decreased arterial pO2 is called Hypoxia (hypo = too little, oxys = stands for oxygen) describes and stimulates the respiratory drive.
Psychogenic hyperventilation
As defined above, hyperventilation describes the state of accelerated and deepened breathing beyond normal requirements. The psychogenically triggered variant is completely detached from the regulatory mechanisms of the body.
The increased breathing means that a lot of CO2 is exhaled and therefore there should actually be a reflex-related decrease in breathing. However, this regulation loop does not work in psychogenic hyperventilation, so that those affected continue to climb into the state of deepened and accelerated breathing with a feeling of shortness of breath. The consequence of psychogenic hyperventilation is a decrease in arterial and alveolar pCO2. This results in a respiratory alkalosis, i.e. a breath-dependent basic state of the blood in the form of an increase in pH value, as the CO2 can no longer lower the pH value through exhalation. So it can be said that psychogenic hyperventilation is an inadequate response, detached from the normal pathophysiological mechanisms of the body.
causes
.jpg)
The triggers for psychogenic hyperventilation are varied and individual. Often the accelerated breathing is related to psychologically stressful situations. Anxiety, depression, aggression, pain stimuli and stress can also be the cause of psychogenic hyperventilation. Affected people are often not aware that their emotional situation is about to provoke hyperventilating. Therefore this happens often unconsciously. According to recent studies, women are more often affected than men. In addition, the risk of psychogenic hyperventilation increases in the second to third decades of life.
Symptoms
The symptoms of psychogenic hyperventilation are often described under the synonym “hyperventilation syndrome”. Despite the increased breathing, the patients have the feeling of shortness of breath, so that they often panic and get even more into the accelerated but also ineffective breathing. The most common symptoms that sufferers report are cold sweats, tremors, panic, dizziness, headache, increased reflexes, chest pain, palpitations, and tachycardia. Usually the symptoms are acute and go away as quickly as they came. However, if it doesn't, it can have more far-reaching effects.
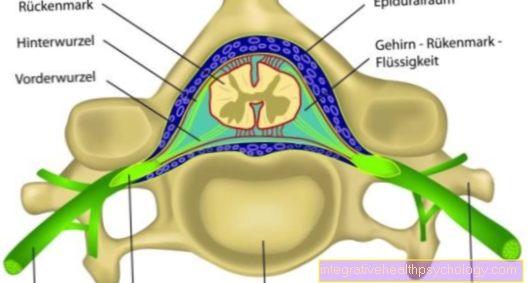
The developing respiratory alkalosis can lead to paraesthesia. This refers to unpleasant sensations in certain areas of the skin, which are usually painless and are often described as "tingling sensations" and "pins and needles". These paresthesias come about as follows: the respiratory alkalosis in the blood causes some proteins to give up their protons and are therefore negatively charged. Now they are able to intercept the doubly positively charged calcium, which circulates in the blood, so that a relative calcium deficiency arises. Relatively because in principle there is still enough or the same amount of calcium, just not available to the body. The calcium deficiency induces tetany (muscle cramps). In extreme cases, the hands may have cramped paws.
In addition to the hyperventilation tetany due to the respiratory alkalosis, the low pCO2 has a particular effect on the vessels in the brain. A high CO2 value, which also implies a low O2 value, leads to vascular dilation so that the brain can be optimally supplied with a lot of blood despite the low oxygen content. The other way around, i.e. in the case of psychogenic hyperventilation and the associated low pCO2, the blood vessels constrict, so that those affected suffer from headaches, dizziness and visual impairment due to the reduced brain perfusion.
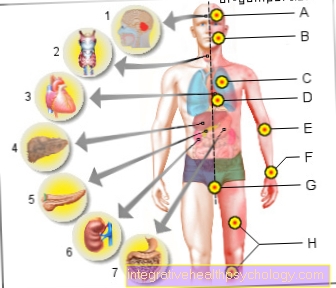
Typical for those affected is nervous behavior with functional complaints such as muscle cramps and visual disturbances, but also gastrointestinal problems and sleep disorders.
In the worst case, a psychogenic hyperventilation attack can lead to unconsciousness.
Diagnosis
Here the clinical signs play a crucial role. Hyperventilation is also used to support the suspected diagnosis Blood gas analysis carried out. Here one expects decreased bicarbonate and CO2 values with mostly increased pH– and O2 values. Basically, the explicit diagnosis of the psychogenic form of hyperventilation is a diagnosis of exclusion. Therefore, problems with the heart (cardiovascular disorders or cardiovascular disorders) and the lungs (asthma) must be excluded. Auscultation findings in the lungs should usually be normal in psychogenic hyperventilation.
therapy
The first priority is always to try to calm the patient down. By consciously breathing in and out, the attack-like hyperventilation can often be brought under control, so that the pCO2 quickly returns to normal and the symptoms quickly subside.
Psychogenic hyperventilation can be brought under control with so-called "bag rebreathing". The patient should hold a plastic bag in front of / over his mouth and try to breathe into it slowly and calmly. The exhaled CO2 content is immediately inhaled again and over time the initial pCO2 drop is counter-regulated again, which compensates for the respiratory alkalosis.It is important that bag rebreathing is only used if you are certain that psychogenic hyperventilation is present. If this were not the case and the patient was breathing too much due to a severe O2 deficiency, this measure would only worsen the situation.
Self-education is advised for patients suffering from a known psychogenic form of hyperventilation. In this way they learn to deal with the situation better and not to panic, but to use bag rebreathing, for example. In addition, it often helps to consciously use diaphragmatic breathing and place your hands on your stomach in order to actively support the breathing movement. Furthermore, it makes sense to regularly perform relaxing exercises and autogenic training to counteract the causes. The more confident a patient feels in dealing with the situation of psychogenic hyperventilation, the less bad the symptoms are and the easier it is to get such an attack under control.
Read more on the topic: Breathing exercises to relax
If the therapeutic measures mentioned do not help, psychosomatic treatment should be considered.
If a patient develops into hyperventilation tetany, diazepam, a muscle-relaxing drug, must be administered in addition to the bag-rebreathing measure.