Non-purulent meningitis
Synonyms in a broader sense
Meningitis, encephalitis, meningoencephalitis
Medical: Serosa menigitis
English: meningitis, encephalitis, brain inflammation, brain-fever
General information
General information on the topic (What is menigitis?) Can be found under our topic:
- meningitis
definition
The term meningitis (meningitis) describes an inflammation (-itis) of the meninges and spinal cord membranes (Meninges), which can be triggered by very different pathogens.
There are two forms of meningitis:
- purulent meningitis (see following text)
- non-purulent meningitis

The purulent meningitis (purulent meningitis) is caused by bacteria. It is associated with a high fever and severe general clinical picture and is an absolute emergency that must be treated immediately.
The non-purulent meningitis (non-purulent meningitis), for that as a rule Viruses are responsible, is usually harmless and often occurs in the context of general virus infections (except for the Herpes simplex encephalitisrepresenting an acute emergency).
The symptoms and the course are milder and the prognosis is better.
Viral meningitis
(= acute, lymphocytic meningitis, simple viral meningitis)
Occurrence and gender distribution
By far the most common form of inflammatory diseases Central nervous system (CNS), i.e. the brain and the spinal cord with its skins and liquor spaces, is viral meningitis (acute, lymphocytic meningitis) with 10-20 cases per 100,000 inhabitants per year. Men are affected slightly more often than women. It is believed that many common infections caused by viruses have mild concomitant meningitis which is not diagnosed.
You have to distinguish them from the rare but dangerous Viral encephalitis, i.e. the acute inflammation of the brain itself or the spinal cord (myelitis, myelon = spinal cord), which in some cases can result from such a slight infection.
Cause and pathogen
The causative agents of viral meningitis have to be divided into two groups:
- into the primarily neurotropic viruses, that is, viruses that primarily penetrate the CNS along nerve roots and have the tendency to settle there and sometimes remain inconspicuous for years (virus persistence, i.e. they exist there without causing symptoms), but they too can cause "normal" viral meningitis (eg the varicella-zoster virus (chickenpox and shingles virus) or the TBE virus) and
- In the non-primarily neurotropic viruses, these are all viruses that preferably cause our colds (“flu-like infection”) in spring and autumn and in most cases get into the meninges (meninges) with the blood and which do not get there either survive (e.g. coxsackie, echo, mumps, measles or adenoviruses). They are the main causative agents of simple viral meningitis. There are regional / local differences with a varying spectrum of pathogens.
In western countries, however, unusual viruses such as the Hantaan virus, the Puumula virus, the Nipah virus, the West Nile virus (WNV) and the Japanese encephalitis virus (JEV) are increasingly found.
Symptoms
Coxsackie and Echovirus infections make up for one Incubation period of 5 to 10 days by flu symptoms such as fever, sniff, Vomit, Sore throat and limbs noticeable.
Then the symptoms of acute viral meningitis set in later. They resemble those of bacterial meningitis with a headache and Neck stiffness, but they are less pronounced, more in the sense of irritation of the meninges.
Often the patients are with clear awareness and have light fever. If the inflammation is due to the brain spreading (meningoencephalitis), focal symptoms can be like a epileptic seizure, speech disorders or Paralysis occur.
In general, however, the symptoms subside after a few days. Here, too, the triggering viruses cannot be distinguished from the meningitis symptoms, but the pathogen can be deduced from the accompanying clinical symptoms. So go for example Echo viruses more likely to have gastrointestinal symptoms like diarrhea along, Coxsackie Viruses with tonsillitis (with Coxsackie B infections, severe Chest pain and a Myocarditis occur) and that Epstein-Barr Virus (EBV, the causative agent of Pfeiffer's glandular fever) with swelling of the spleen and lymph nodes.
diagnosis
If viral meningitis is suspected, as with bacterial meningitis, an examination of the nerve water is sought with the help of the CSF puncture on.
In contrast to the purulent, bacterial meningitis Only a few impressive changes: The puncture has a clear to slightly cloudy color, as the number of cells is increased, but often does not exceed 1500 cells.
These are also not pus-forming cells (Granulocytes) as in purulent meningitis, but rather Lymphocytes (White blood cells).
Lymphocytes are the cells of our immune system that fight viruses and therefore do not form pus.
Protein, sugar and lactate - other important markers of the nerve water - have almost normal values, as does the procalcitonin in the blood (always below 0.5 ng / ml), which is a sensitive marker for differentiating between purulent and non-purulent meningitis (only increased with purulent).
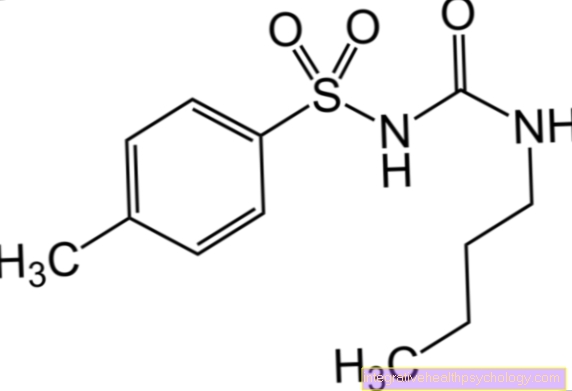
The identification of the pathogen is best done by detecting the specific antibody in the blood with the help of ELISA-Technology (enzyme-linked immunosorbent assay). If the proof is unsuccessful, the will also find PCR (Polymerase chain reaction) Application.
The PCR directly detects the DNA, i.e. the genetic material of the viruses, and is now used as a routine method for the detection of certain viruses, especially the herpes virus group (HSV, VZV, CMV, EBV), but also for the HI virus and others.
Therapy and prognosis
A simple viral meningitis, like simple, viral meningoencephalitis, does not require any special therapy. Bed rest, possibly antipyretic medication (e.g. paracetamol) and painkillers as well as stimulus shielding are useful. The prognosis is good. Permanent damage is not to be expected.
Vaccination / prophylaxis
For some viruses that can potentially affect the brain and meninges, vaccination in childhood is the best prophylaxis. These include measles, rubella, mumps, chickenpox (varicella) and poliomyelitis viruses (the causative agent of polio).
The virus is only vaccinated against the causative agent of early summer meningoencephalitis, the TBE virus, when traveling to the corresponding risk areas (especially southern Germany, but the virus is spreading further and further north), as is the case with the Japanese encephalitis virus.
Also read our topic: Vaccination against Japanese encephalitis
Chronic lymphocytic meningitis or (meningo-) encephalitis
Cause and pathogen
The causative agent of this form of the Meningitis are usually not viruses, but
- Mushrooms (e.g. Cryptococcus, cryptococcal meningitis / encephalitis),
- Parasites (e.g. Toxoplasma, toxoplasmosis, Pathogens are transmitted through cats)
- the tuberculosis pathogen (Mycobacterium tuberculosis, tuberculous meningitis) and other mycobacteria
- Bacteria like that Borrelia (Borrelia burgdorferi, Borreliose, Pathogens are transmitted by ticks) or the pathogens of the syphilis, Treponema pallidum (neurolues, neurosyphilis)
- and other.
In addition to Lyme disease, they often occur in poor countries, in people infected with HIV and other patients with a weakened immune system and manifest themselves with a slow decline in personality, disorders of attention and memory and increasing neurological deficits.
The number of cells in the nerve water (liquor) is not or only slightly increased.
At the time of diagnosis, in contrast to acute (fresh) processes, antibody production can often be found within the Liquor spaces detect (intrathecal immunoglobulin synthesis).
The antibodies against a virus are then more highly concentrated in the cerebral fluid than in the blood, which suggests that they are within the central nervous system (CNS) a slowly growing process is taking place.
Summary
The pathogen-related, non-purulent inflammatory processes in the central nervous system (meningitis, Encephalitis, Meningoencephalitis) can be classified as follows:
- viral (acute lymphocytic, serous) meningitis
- non-viral (chronic lymphocytic) meningitis
- acute viral encephalitis
An inflammatory process caused by viruses should always be considered if the following factors can be found in the medical history (anamnesis):
- Viral diseases in the area (e.g. mumps, chickenpox, polio)
- Insect or Tick bites (e.g. TBE virus, borrelia (borreliosis)
- Animal bites (e.g. Rabies)
- After blood transfusions or organ transplants (e.g. HIV, hepatitis A, hepatitis B, hepatitis C virus, Cytomegalovirus (CMV), Parvo virus B19 (Causative agent of Ringlet rubella))
- Immunodeficiency caused by cancer, medication (e.g. rheumatism or rheumatoid arthritis) or AIDS (e.g. CMV, Varicella zoster virus (VZV)
- Stays abroad